As a result of our complex and fragmented healthcare system, patients often experience delays in care. Nurse navigators offer individualized support to patients while alleviating barriers and ensuring timely access throughout the cancer care continuum. The oncology nurse navigator (ONN) is uniquely positioned to advocate and facilitate seamless care transitions before, during, and after completing each phase and modality of treatment. As referenced in the book Team-Based Oncology Care, Shockney1 highlights that “the ONN becomes a trusted advocate while providing emotional guidance and ongoing support throughout the cancer trajectory.” The altruistic approach to a successful oncology nurse navigation program is to assess individual patient needs, remove barriers, facilitate timely access to care and resources, and educate and provide emotional support.1
Oncology nurse navigators must demonstrate strong interprofessional communication skills to foster the flow of pertinent information while serving as the liaison among healthcare team members.
To avoid unnecessary delays and negative consequences, the ONN must work fluidly across all 3 domains—diagnosis, treatment, and survivorship—to ensure the patient is informed, empowered, and engaged in their care. Shockney highlights that “poorly coordinated care transitions and inadequate communication between healthcare providers can lead to poor patient outcomes.” ONNs must demonstrate strong interprofessional communication skills to foster the flow of pertinent information while serving as the liaison among healthcare team members. Collaboration and coordination among primary care providers, oncologists, specialists, and other members of the team are essential for patients to receive quality and timely cancer care.1
Problem Description
An ONN identified an opportunity for improvement based on witnessed inefficient, duplicative, and inconsistent workflows for newly diagnosed patients with lung cancer. The frequency of fragmented care was in part due to varying referral patterns, inconsistent sequence of care, and lack of a consistent point person for referrals. The nature and significance of the local problem led to an opportunity for ONN involvement at the time of confirmed lung cancer diagnosis. For example, when a patient is referred by the thoracic surgeon, there is a seamless transition to oncology through direct notification to the ONN upon confirmed malignancy. However, patients who enter from a primary care referral often experience a delay in care based on the sequence of events leading up to the initiation of treatment.
Available Knowledge
Lung cancer care requires a multidisciplinary team approach with thoughtful and effective coordination and communication across multiple disciplines, including primary care, radiology, pulmonology, medical oncology, radiation oncology, and surgery.2 According to the literature, time to treatment (TTT) is considered a quality indicator for cancer care, but it is not well defined. TTT is difficult to quantify based on the complexity of the diagnostic process and treatment decisions depending on the stage, performance status, and quality of life (QOL).2
Recently, TTT has been defined as the total number of days from the date of diagnosis to the first day of treatment.3
In a scoping review of the literature, Jacobsen et al2 recommended that diagnosis to treatment wait interval metrics are needed to evaluate and improve the timeliness of care. Delays in diagnosis and treatment of lung cancer can result in significant emotional distress, diminished QOL, and increased use of healthcare resources.4
To reduce delays in care, various organizations have published consensus-based standards to offer recommendations for timely lung cancer care. Upon review of the literature, the guidelines are inconsistent and conflicting. The British Thoracic Society first published guiding principles in 1998, recommending a maximum diagnosis to treatment interval of 8 weeks for surgery, 7 weeks for radiation, and 4 weeks for chemotherapy once diagnosed.2 In 2000, the RAND Corporation formulated US-based guidelines of target intervals for access to care, although there are no federal standardized guidelines regarding timeliness to care. With a focus on quality indicators, the RAND criteria recommend confirmation of diagnosis within 2 months after suspected lung cancer and treatment offered within 6 weeks after diagnosis.5 In 2011, the National Institute for Health and Care Excellence in the United Kingdom published revised guidelines, recommending that patients with suspected lung cancer receive a specialist appointment within 14 days and start treatment within 28 days from referral.2
In 2015, the Institute of Medicine, now called the National Academy of Medicine (NAM), released a report calling for an increased understanding of and focus on timely care.6 According to the NAM, timeliness to care is considered a fundamental component of high-quality healthcare. Unfortunately, these standards are not consistently maintained, and as a result, delays in lung cancer care persist. To move the needle with timeliness to treatment, the root cause of such delays needs to be better defined. For example, is the nature of the delay patient- or system-based?
In a systematic review by Zhang et al, interventions were validated to reduce time intervals, including fast-access diagnosis programs, patient navigation, and multidisciplinary strategies.7 They also highlighted the inconsistent variations in interval definitions and the association between times to diagnosis and treatment and patient outcomes. In addition, they substantiated the limitations of an analytic approach that fails to account for a potential waiting time paradox where patients are treated faster when presenting with more severe symptoms due to disease progression.7 This phenomenon is reinforced in a population-based study as the sicker quicker effect.4
Gomez et al performed a retrospective population-based study to evaluate predictors of treatment delay. The study found that the median diagnosis to treatment interval was 27 days. In alignment with the national benchmark, a diagnosis to treatment interval of fewer than 35 days is associated with improved survival for patients with localized disease.8 One common treatment delay identified was obtaining a timely PET/CT. A benchmark of a 7-3-10–day interval time frame was recommended, with the goal of 7 days from diagnosis to PET, 3 days from PET to follow-up, and 10 days to subsequent treatment start, to improve adherence to timely treatment.8 With the constraints of our current health system and often limited access to care, is this recommendation realistic? Vidaver et al published a multisite, US-based study to explore when and why delays occur in lung cancer care.3 Possible reasons for delay include lack of communication of positive radiologic findings to primary care provider and/or patient; clinical delays due to other health conditions; and system factors, such as delays in scheduling tests or specialist visits. The study documented a 52-day median time to treatment from the first presentation or suspected lung cancer diagnosis. Based on a review of the literature, a recommendation of a 52-day maximum TTT was documented as a desirable interval for treating patients with lung cancer.3
To reduce delays in care, organizations have published consensus-based standards to offer recommendations for timely lung cancer care. Upon review of the literature, the guidelines are inconsistent and conflicting.
In a retrospective review to evaluate access to care and the timeliness of the care received in non-navigated and nurse-navigated cohorts, researchers found that nurse navigation implementation improved access and timeliness to lung cancer care.9 The nurse navigator assumed 2 primary responsibilities: expedite diagnostic procedures and facilitate specialty consultations. For the non-navigated cohorts, the time between suspicion of cancer to treatment was 64 days, and after the implementation of nurse navigation, the time was reduced to 45 days (P<.001).9 This review demonstrated the nurse navigators’ ability to streamline the diagnostic process, provide patient support and education, and coordinate the sequence of specialty consultations with medical and radiation oncology.9
In another retrospective study, Albano et al aimed to evaluate the duration of time to diagnosis and first treatment and investigate reasons for delays in care. The authors suggested “a coordinated multidisciplinary lung cancer program may reduce delays in care, thereby improving patient outcomes.”10 As demonstrated in a published abstract through the Academy of Oncology Nurse Navigators, the ONN facilitated timely intervention by obtaining an appointment with the appropriate oncology provider. As a result, patients experienced increased coordination and less fragmented care, leading to decreased diagnosis and treatment times.11 In a systematic literature review, Vinas et al reinforced that ONNs are uniquely positioned to harmonize diagnostic workup and the subsequent timing of appointments, optimizing adherence to timely treatment.12 In the Clinical Journal of Oncology Nursing, Hunnibell highlighted that cancer care coordination with dedicated nurse navigators resulted in a measurable improvement in timelines to care.13 Shockney highlights that ONNs are instrumental in facilitating care transitions to mitigate gaps in care delivery and that “they bring a unique and powerful perspective to the patient’s care as there is oversight of the patient’s comprehensive care needs across the care continuum and care settings interfacing with the multidisciplinary care teams.”1
An in-depth literature review suggests that communication, collaboration, and laterally integrated care coordination are essential cornerstones to delivering efficient, timely, and patient-centered cancer care. Although defining benchmark intervals for timely care remains a limitation, the literature supports the premise of the opportunity for quality improvement.
Global Aim
The purpose of this quality improvement (QI) project is to remove barriers and facilitate timely access to care with the implementation of a referral to an ONN at the time of diagnosis. In support of best demonstrated practice, the ONN will anticipate needs and offer streamlined communication with the multidisciplinary team to confirm the sequence and timing of referrals and anticipated diagnostic imaging and procedures.
Specific Aim
The specific aim was to decrease the TTT, measured in days, from 21 days to 14 days from initial consult to initiation of treatment by July 1, 2022, with the implementation of a standardized thoracic oncology clinical pathway supporting referral to an ONN at time of diagnosis.
Methods
A 5Ps (purpose, patients, professionals, processes, and patterns) microsystem assessment was used as the framework to understand the evidence of the problem. The Plan-Do-Study-Act (PDSA) quality improvement and evidence-based practice model was used to assess the value of the intervention through a series of ongoing cycles.
Data collection with an Excel spreadsheet, initiated by the ONN, was used to quantify the time of diagnosis to consult and time of initial consultation to treatment. A robust Excel spreadsheet data analysis was completed with applied formula extrapolation to quantify the length of time from the initial consult to the initiation of treatment.
Intervention(s)
A thoracic oncology pathway was created to define a standardized algorithm for patients newly diagnosed with lung cancer (Figure 1). To align processes, a referral was initiated via staff message or communication during our biweekly thoracic tumor board meeting. The process redesign was implemented to achieve a more efficient workflow across the cancer care continuum when referring a patient to oncology from thoracic surgery. The primary barrier from the lens of the thoracic surgeon was the lack of a primary point person for referrals to oncology, resulting in a delay in initial consult and subsequent treatment.
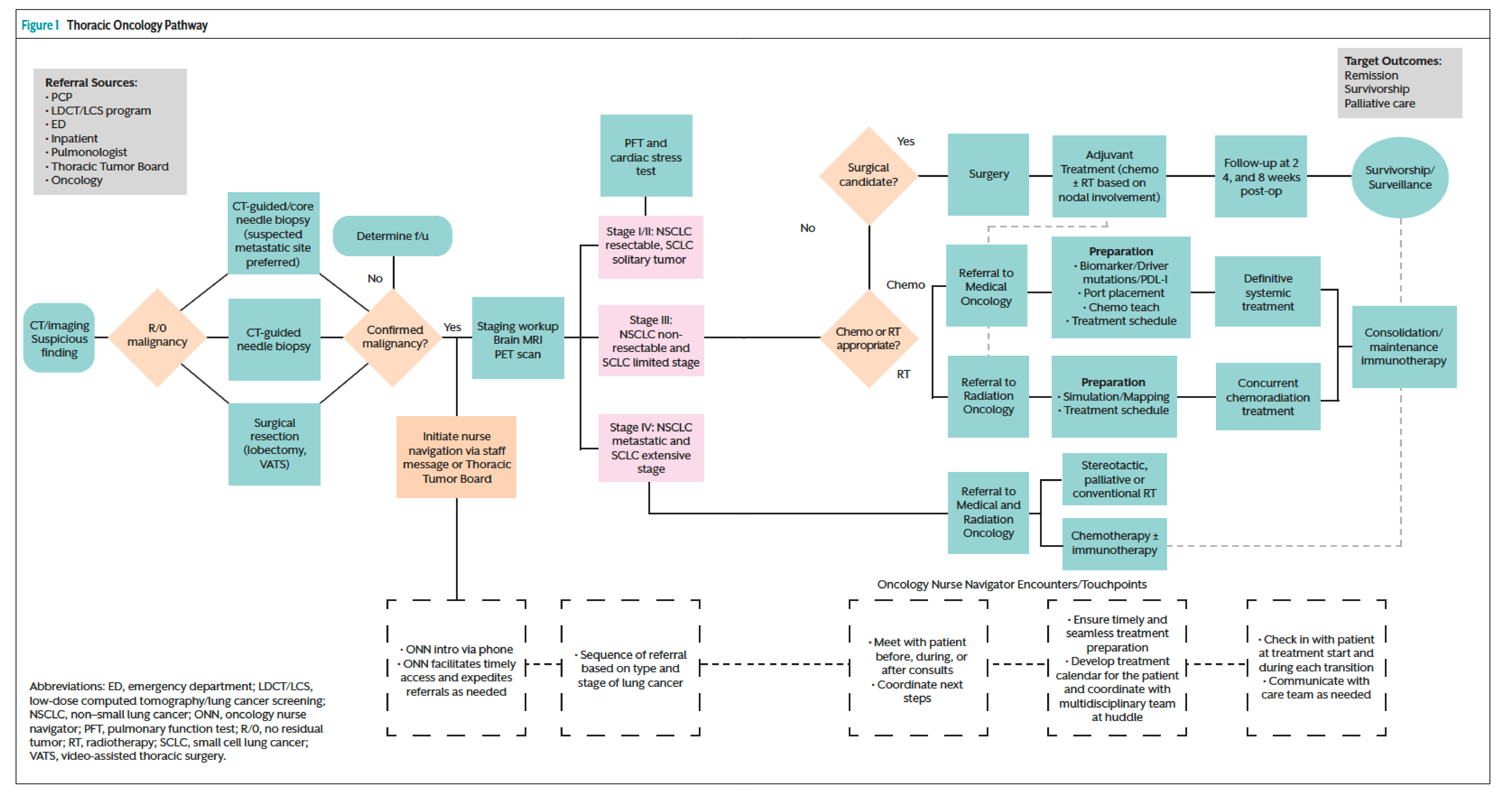
Involving the ONN upstream at the time of diagnosis offers expedited and thoughtful care coordination upon referral to the cancer center (ie, medical oncology or radiation oncology). Furthermore, the ONN can facilitate additional staging/diagnostic testing (ie, PET/CT scan and brain MRI) necessary to determine the extent of the disease and treatment recommendations before the initial oncology consult.
ONNs can offer a personalized, patient-centered approach while facilitating timely access to care, alleviating barriers, and advocating for patients. When orchestrating complex care, the ONN is the main point of contact to coordinate care, offer support, validation, and patient empowerment while also ensuring seamless transitions by eliminating unnecessary gaps along the care continuum. They also serve as fierce advocates, guiding patients to informed/shared decisions with the care team while seeking to understand patient wishes, values, and priorities. As the primary point person for communication, the ONN can ease the fear of the unknown during a vulnerable and often overwhelming time for the patient.
The process concludes with the initiation of treatment (systemic, targeted, stereotactic, conventional radiation, or palliative treatment). Implementation of this workflow is expected to improve the timeliness of consultation, remove barriers to care, and decrease the time from consultation to initiation of treatment. As a result of expediting access to care, we hope to address various key performance indicators such as quality, timeliness, and improved patient experience.
For this QI project, the key stakeholders include members of our thoracic surgery, radiation oncology, medical oncology, and pulmonology teams, and the primary care ambulatory care coordinators. Communication and collaboration with the care team remain paramount as we determine a framework for the proposed pathway. Ensuring a multidisciplinary approach will prove advantageous for the success and implementation of the thoracic oncology pathway.
Study of the Intervention(s)
To assess the impact of upstream oncology nurse navigation and to determine if the observed outcome resulted from the creation of a thoracic oncology pathway, a retrospective chart review was completed. After review of the collected data from July 1, 2021, to June 30, 2022, we quantified various metrics, including date of biopsy, date of initial consult, date of treatment initiation, and point of entry/referral, to determine if an improvement in timeliness to care occurred. An Excel spreadsheet formula was created to measure data entry intervals.
Measures
The expected outcomes for this project include a decrease in the average TTT interval as well as a refinement of the workflow process with upstream involvement of the ONN.
For purposes of this PDSA cycle, data collection from June 1, 2021, to June 1, 2022, was analyzed to quantify the benefits of upstream oncology nurse navigation. A total of 130 patients with lung cancer were navigated during this time frame. A retrospective chart review identified that 40% (n=52) of the patients navigated entered through thoracic surgery. When determining other points of entry, 26% of the patients entered through medical oncology (n=34), 19% through radiation oncology (n=25), 7% through inpatient RN case managers (n=9), and 8% other (n=10) (Figure 2). This demonstrates an opportunity to capture patients who do not enter through thoracic surgery at the time of diagnosis versus initial consult
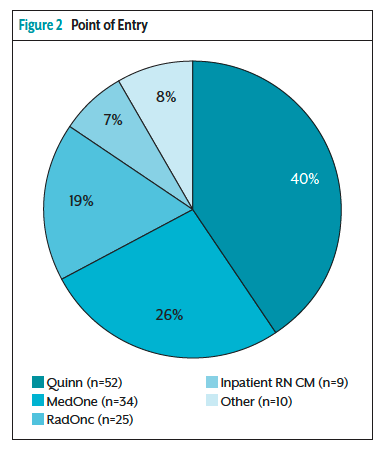
During the Do phase of the QI project, we added the referral source to the categorical data collection to further refine the point of entry and evaluate the impact navigation had on TTT. The point of entry was categorized as a thoracic referral or other referral, to measure the TTT based on when the ONN became involved.
To assess the impact of upstream oncology nurse navigation and to determine if the observed outcome resulted from the creation of a thoracic oncology pathway, a retrospective chart review was completed.
Outcome Measures
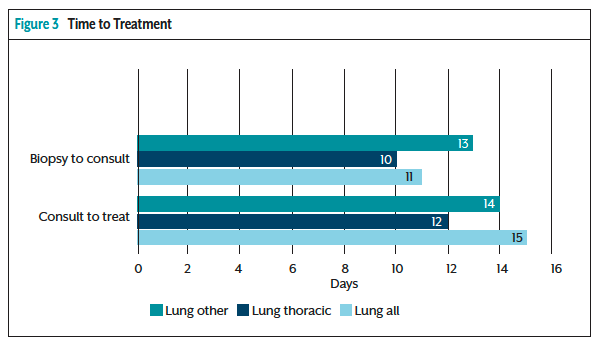
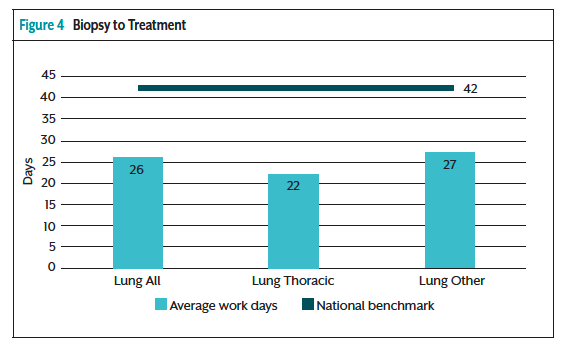
As a result of the implementation of upstream nurse navigation, the outcome measures showed a 3-day decrease from the diagnosis to consult and a 2-day decrease from consult to treatment based on where a patient entered the system (Figure 3). An in-depth analysis revealed that ONN involvement improved time from biopsy to initial consult by 18% compared with patients who did not have an ONN facilitating a timely referral and subsequent consult. Another key finding of the collected data demonstrated that the average length of time from the biopsy to treatment initiation for all lung cancer patients navigated was 25 days, compared with the national benchmark to offer treatment within 42 days of initial diagnosis (Figure 4). Despite not having a benchmark for TTT specific to ONN involvement pre- and postimplementation of the program, we are setting the bar by initiating treatment almost 2 weeks sooner when compared with the national TTT recommendation.
Process Measures
Two contextual elements that stood out as the cornerstones of this quality improvement are processes and professionals. Standardizing the process of upstream oncology nurse navigation and effective interprofessional collaboration are vital to the success of improving timeliness to treatment. Improved patient experience and outcomes remain the primary focus of the interventions. A cause and effect diagram assisted in determining the contributing factors of delayed treatment.
Analysis
To evaluate this QI proposal’s anticipated outcome, we analyzed both categorical and continuous data collected from the implementation of the thoracic oncology pathway. We used descriptive statistical analysis of categorical data with frequency and percentage reported, and continuous data reported as mean, standard deviation, and range.
We seek to understand and validate a positive correlation between upstream nurse navigation and timeliness to treatment by analyzing the data via inferential statistical analysis. An Excel spreadsheet was developed for timely and efficient data collection reported monthly. The columns are organized by the following categories: patient name, medical record number, site, diagnosis, date of biopsy, date of medical oncology consult, date of radiation oncology consult, date of first treatment start (surgery, radiation treatment, or systemic treatment), and the referral source or point of entry.
The rationale for choosing TTT intervals as the focus for this quality proposal is based on the specificity of real-time continuous data collection, including validity and reliability. Consistent and accurate data collection, with a customized Excel spreadsheet, will be used to extrapolate the data into quantifiable metrics. Correlational analysis tools were investigated to quantify a linear relationship between 2 variables.
Results
As a result of an interprofessional partnership with the thoracic team, the upstream system-based pathway enabled the ONN to connect with the patient upon initial diagnosis of lung cancer to offer emotional support and seamless coordination of care. Although the specific aim of decreasing the time from initial consult to treatment by 7 days was not achieved, the key findings demonstrated a 5-day decrease in time to treatment. Based on the categorical data, the mean and percentage of thoracic referrals represented 40% (n=52) of the total patients navigated (N=130). The point of entry or referral source was an unexpected influence on context and warrants future PDSA cycles focused on decreasing the time to treatment for patients entering through primary care, where the longest time to treatment interval was observed.
Discussion
Interpretation/Limitations
An unintended consequence experienced during the analysis stage was the variability of the collected data. Variables such as patient-related delays to care, inability to obtain biopsy, and previously established patients made it difficult to aggregate time intervals and analyze the data to quantify the benefits of upstream oncology nurse navigation.
Efforts made to minimize and adjust for the above limitations were accomplished by reviewing outliers in the continuous data to actualize the internal and external validity with the date of biopsy, consult, and treatment to determine if the ONN had a confounding impact on the average time interval to treatment. In other words, if the ONN did not have an impact on the timing of initial diagnosis to consult or consult to treatment, then a “n/a” was documented for that metric and omitted from the interval analysis. These unintended variables made it difficult to succinctly quantify an improvement and tell the intended story when reporting the results of the implementation.
Conclusions
As referenced in the Journal of Quality Improvement, a seamless, patient-centered experience across the care continuum is the goal of high-quality and efficient care.14 This statement echoes the core themes for a proposed pathway to highlight care excellence and best demonstrated practice within the clinical microsystem. As the complexity of cancer treatment and the healthcare landscape evolves, patient-centered care and collaboration remain essential components of a successful microsystem.
As the primary point of contact across the care continuum, ONNs aim to close communication gaps and facilitate comprehensive, patient-centered care while advocating informed/shared decisions with the care team. ONNs are uniquely positioned to provide individualized support to patients and communicate anticipated next steps to ease the fear of the unknown—supporting the notion of upstream is the dream of ONNs. Implications for practice are paramount as the complexity of cancer care continues to evolve.
Acknowledgments
I would like to thank my distinguished colleague, Danielle Revoyr, MBA, MS, RDN, LD, CSO, CNSC, for sharing her expertise in data analytics and Excel extrapolation to quantify the results of this QI project. I would also like to express my sincere gratitude to my mentor and capstone preceptor, Marsha Clements, PhD, RN, OCN, NEA-BC, for her ongoing support, guidance, and encouragement to pursue my master’s degree and believing in my ability to help build the oncology nurse navigation program.
References
- Shockney LD. Team-Based Oncology Care: The Pivotal Role Of Oncology Navigation. Springer; 2018.
- Jacobsen MM, Silverstein SC, Quinn M, et al. Timeliness of access to lung cancer diagnosis and treatment: a scoping literature review. Lung Cancer. 2017;112:156-164.
- Vidaver RM, Shershneva MB, Hetzel SJ, et al. Typical time to treatment of patients with lung cancer in a multisite, US-based study. J Oncol Pract. 2016;12:e643-e653.
- Forrest L, Adams J, White M, Rubin G. Factors associated with timeliness of post-primary care referral, diagnosis and treatment for lung cancer: population-based, data-linkage study. Br J Cancer. 2014;111:1843-1851.
- Bukhari A, Kumar G, Rajsheker R, Markert R. Timeliness of lung cancer diagnosis and treatment. Fed Pract. 2017;34(suppl 1):24S-29S.
- National Academies of Sciences, Engineering, and Medicine. Improving Diagnosis in Health Care. National Academies Press; 2015.
- Zhang J, IJzerman MJ, Oberoi J, et al. Time to diagnosis and treatment of lung cancer: a systematic overview of risk factors, interventions and impact on patient outcomes. Lung Cancer. 2022;166:27-39.
- Gomez DR, Liao K-P, Swisher SG, et al. Time to treatment as a quality metric in lung cancer: staging studies, time to treatment, and patient survival. Radiother Oncol. 2015;115:257-263.
- Kunos CA, Olszewski S, Espinal E. Impact of nurse navigation on timeliness of diagnostic medical services in patients with newly diagnosed lung cancer. J Community Support Oncol. 2015;13:219-224.
- Albano D, Bilfinger T, Feraca M, et al. A multidisciplinary lung cancer program: does it reduce delay between diagnosis and treatment? Lung. 2020;198:967-972.
- Fox-Kay K, Childress C. How coordination of care along the diagnostic continuum improves timeliness to care for lung cancer patients. Journal of Oncology Navigation & Survivorship. 2020;11(11):398.
- Vinas F, Ben Hassen I, Jabot L, et al. Delays for diagnosis and treatment of lung cancers: a systematic review. Clin Respir J. 2016;10:267-271.
- Hunnibell LS. Using nurse navigation to improve timeliness of lung cancer care at a veterans hospital. Clin J Oncol Nurs. 2012;16:29-36.
- Nelson EC, Batalden PB, Huber TP, et al. Microsystems in health care: Part 1. Learning from high-performing front-line clinical units. J Qual Improv. 2002;28:472-493.



