Kristin L. Soper, DNP, MS, RN, ANP-BC, AOCNP
Susan Tiffany, BS, RN, OCN
Upstate Cancer Center, Syracuse, NY
Background
The need for cancer survivorship involvement was extensively discussed in the 2007 Institute of Medicine Implementing Cancer Survivorship Care Planning report.1 Per the National Cancer Institute, as of January 2022, it is estimated that there are 18.1 million cancer survivors in the United States. This population of survivors represents 5.4% of the population. By 2032, the number of cancer survivors is anticipated to increase by 24.4% to 22.5 million and is then projected to grow to 26.0 million by 2040.2 This substantial increase is likely multifactorial, but new and innovative treatment options as well as the advancement made in early detection and diagnostics are definite factors.3 This expected growth supports the continued need for Survivorship resources and support being provided to oncology patients.
Patients eligible for the Survivorship program include analytic patients diagnosed or treated for all or part of their initial course of therapy with curative intent at our institution for stage I, II, and III cancers.
Living through a cancer diagnosis and subsequent treatment typically represents a life-changing event, often including residual and long-term emotional, physical, and psychological components, making it a form of trauma.3 After completion of their therapy, many oncology patients are transitioned to a survivorship program for long-term follow-up care. A survivorship program aims to support patients through these residual effects of diagnosis and treatment by supporting them with wellness strategies as well as bridging the gap between their oncology team and primary care provider (PCP). During treatment, survivors tend to form a close relationship with their oncology-specific teams and then, at times, have difficulty transitioning back to the care of their PCP.4 PCPs are also noted to respect the relationship between patients and their oncology teams and have, in some cases, resisted accepting oncology patients back into their care.4 This is likely due to many factors but can be specific to their lack of oncology training and time restrictions.3
Our institution developed a Survivorship program run almost entirely by an RN navigator. The purpose of the creation of this RN navigator–driven Survivorship program was to ease this survivor transition period and provide improved support and direction to cancer survivors as they evolve past treatment and back into their everyday life. At this institution, survivorship is defined as encompassing guideline-based surveillance for relapse; screening recommendations for second cancers; evaluation, management, and referral for late effects of cancer-directed therapy; and coordination with the medical team to ensure seamless care delivery. Patients eligible for the Survivorship program include analytic patients diagnosed or treated for all or part of their initial course of therapy with curative intent at our institution for stage I, II, and III cancers. For breast cancer cases this includes stage 0 as well.
The Survivorship program was previously run by an advanced practice nurse (APN), but when the position was vacated, the decision was made to transition this program to being RN led. It was determined that much of the previous APN’s efforts fell under the umbrella of RN responsibilities, and while it was convenient to have an advanced practice provider able to easily place orders, it was a difficult position to justify related to the underdevelopment of the program and this role. This Survivorship program serves patients of all ethnicities, ages, and demographics, and although most patients have a diagnosis of breast cancer, the program serves patients with all cancer diagnoses and continues to expand its reach with community outreach and provider education. It was determined that the RN must have clinical knowledge related to expected chemotherapy side effects, surveillance planning, and monitoring and therefore must be, at a minimum, of an RN level. Specific oncologic experience is necessary to appropriately manage this patient population.
Methods
Multiple new interventions initiated by the RN leading this program were implemented to optimize the services offered to survivorship patients. The Survivorship program was adjusted to be an RN-driven program in 2022; this was post-COVID when the program was being redefined after telemedicine visits became more mainstay in the oncology world. Initiatives included improvement of the survivorship encounters, the creation of a PCP letter, and survivorship-specific electronic medical record (EMR) documentation options, as well as a patient survey.
Survivorship Encounters
The Survivorship RN navigator connects with appropriate patients via telephone within 6 weeks of treatment completion, then 6 months later, and finally annually. Patients are triggered to be appropriate for survivorship after the completion of specific treatment plans and referrals are placed by care team providers. Six weeks after the completion of treatment was a decided-upon interval to ease that transition period and to ensure that the patient had the appropriate resources in place posttreatment. This is also noted to be a time when the patient can struggle emotionally and feel “out of place” in their cancer journey.3 As patients ease back into their day-to-day life, the Survivorship RN can provide education and support at the 6-month and annual intervals. The focus of these visits is on needed pertinent surveillance, overall wellness, available resources, healthy eating habits, and physical activity. The patients are all internally referred by their primary medical oncology, radiation oncology, or surgical oncology teams. The Survivorship RN navigator completes these visits by telephone call because previous feedback included patients not wanting or being able to come back in person for another appointment. If patients shared that they preferred to be seen in person, this could then be arranged. During these interactions, the Survivorship RN navigator discusses additional community resources and both internal and external referral options. Examples of on-site resources include nutrition, psycho-oncology program, financial counseling, lymphedema clinic, speech therapy, Reiki, and smoking cessation. Available off-site resources include massage, acupuncture, light therapy, sex counseling, and chiropractic care.
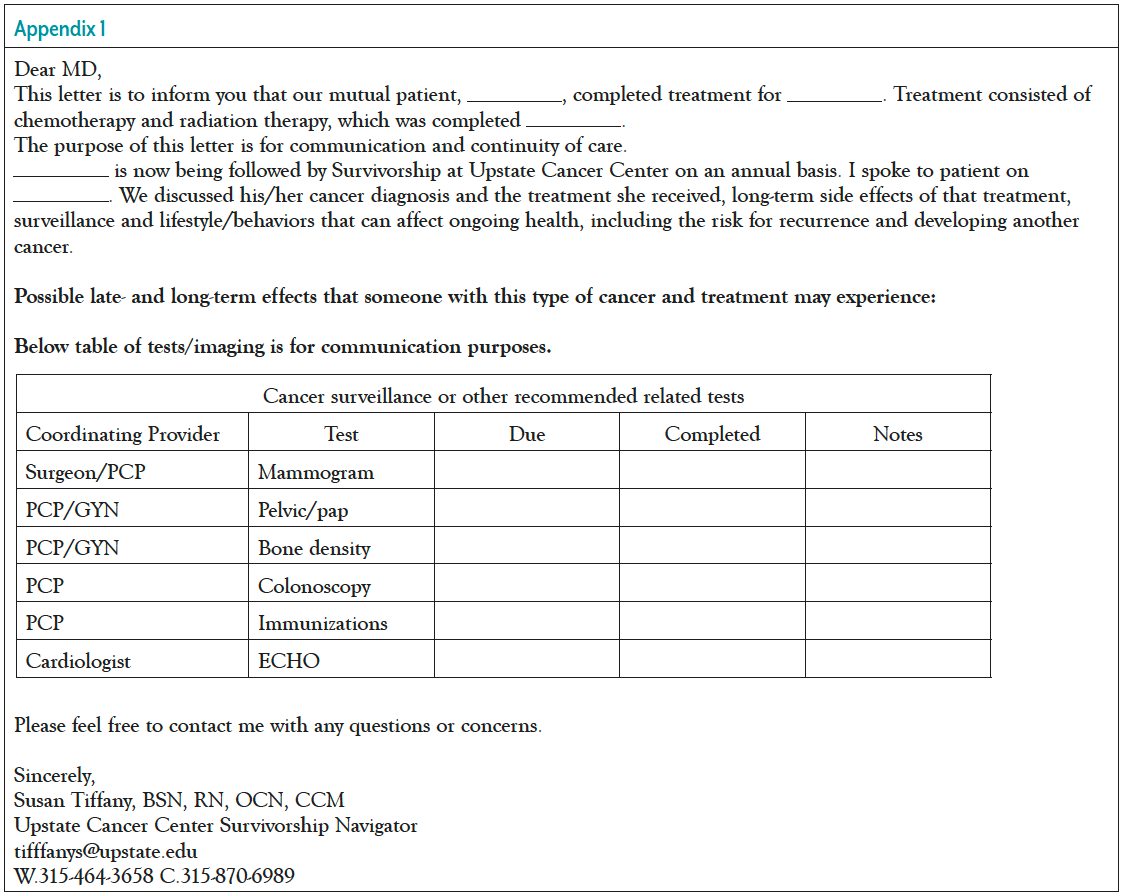
PCP Letter
To assist in filling the gap between PCPs and the oncology team, the Survivorship team created a templated letter for each PCP with personalized patient information (Appendix 1). The letter contains information pertinent to diagnosis, treatment, potential side effects, and needed surveillance and screening testing. The purpose of the personalized survivorship letter from the Survivorship team to the PCP was to ease this transition period, and to provide personalized surveillance and care guidelines to the PCP to properly care for the survivor. The goals of this initiative were to enhance continuity of care, to improve the relationship between oncologist and PCP, to ease the transition from oncologist to PCP, to ensure appropriate screening and surveillance for the patient specific to their cancer treatment plan, and to list potential complications/side effects from past treatment so that the PCP may tailor their care. Previous research indicates that Survivorship teams should clearly specify follow-up recommendations and screening needs that should be completed by the PCP for oncology patients. With the sharing of the survivorship letter to the PCP, the aim was that PCPs would be more confident and prepared to ensure appropriate follow-up care for their cancer patients. Written survivorship care plans have been regarded by both oncologists and PCPs as helpful but not sufficient to ease the transition; the addition of this letter aims to fill this gap to ensure a more comprehensive and thorough transition.
Multiple new interventions initiated by the RN leading this program were implemented to optimize the services offered to survivorship patients. The Survivorship program was adjusted to be an RN-driven program in 2022.
Encounter Documentation
The Survivorship RN navigator noted a need for a specific encounter documentation option in our EMR for survivorship. Previously, this RN navigator would enter the visits as telephone encounters. In addition, this RN navigator noted a need for a specific survivorship assessment in the EMR system. This would take the place of recreating and avoid typing a thorough survivorship telephone encounter.
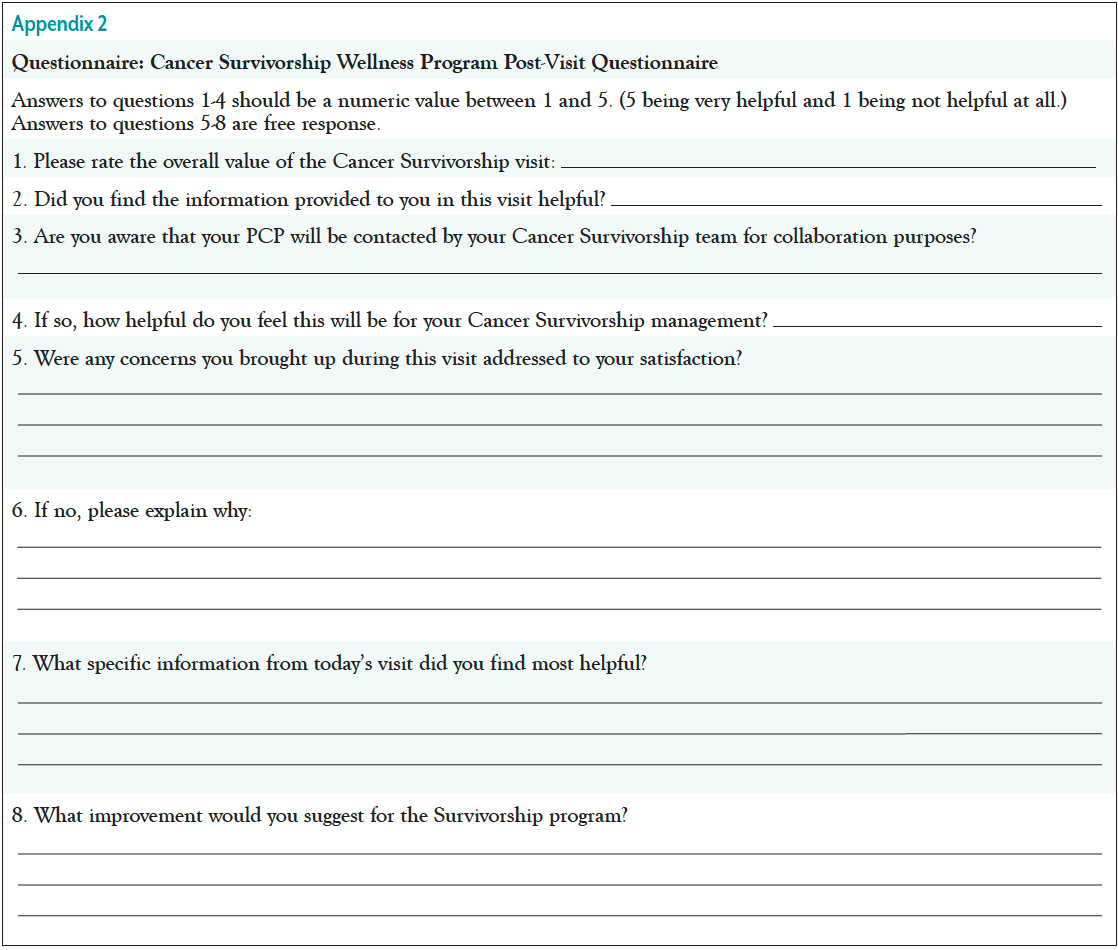
Patient Survey
A survivorship patient survey was created to obtain feedback related to changes being made with the RN navigator–driven Survivorship program. The survey was sent via the patient’s EMR and asked questions pertaining to how helpful the visit was for the patient, as well as if the patient was aware of the connection between the Survivorship RN navigator and their PCP. Additional questions were specific to what was discussed during the survivorship visit, what was most helpful, and what improvements would be helpful to continue to grow this program. See Appendix 2 for additional details pertaining to the patient survey. This survey was created after the interventions were implemented to gauge how the patients were responding to the new program.
Results
Survivorship encounters have steadily increased between 2022 and 2023. The first 3 months of 2022 had 38 encounters compared with 65 in the first 3 months of 2023, an increase of 71%.
The changes implemented thus far have been shown to increase the number of patients being impacted by this program and to increase the collaboration between the oncology teams and the PCPs.
Out of 28 completed surveys, 27 patients found the RN navigator survivorship visit either “helpful” or “very helpful.” Twenty-five of the 28 surveyed patients were aware of the collaboration between Survivorship and their PCP. The majority (92.85%) of these patients did find this collaboration helpful. Other key themes identified in these surveys were that the patients appreciated learning about medication side effects as well as learning about both internal and external resources and the plan for ongoing survivorship support. The patients also stated that they appreciated learning about diet, exercise, and overall wellness. In addition, patients appreciated a full medication review and shared that they appreciated “being heard” and that “someone wanted to hear their cancer journey.” Many also noted the helpfulness of the coordination of care taking place with their other care teams. Improvement suggestions included the option to meet more often and in person. The Survivorship RN shared that her experience with the new EPIC assessment as well as the survivorship encounter type allowed for a more seamless visit and communication among interdisciplinary teams.
Discussion
As the Survivorship RN navigator has worked to optimize her responsibilities as well as the EMR as it pertains to survivorship, the workflow has gradually improved. The ability to easily note in the EMR if a patient is currently being seen by Survivorship is immensely helpful to the interdisciplinary teams involved in care. Now, instead of “telephone encounter,” the EMR clearly notes “SVS,” short for Survivorship. There is now increasing referrals to our internal services, such as nutrition, psycho-oncology, and financial counseling. The Survivorship team is building stronger relationships with external services to offer additional external resources to this patient population. The institution is also much more aware of what services and resources the patients require throughout their survivorship journey. PCP offices have reached out and shared how helpful the survivorship letter is in bridging the gap between the oncology team and the PCP care team. The goal is that with continued collaboration and communication, patients will experience less of a gap in care and more continuity and follow-through with obtaining all necessary side effect management and image monitoring as required.
Concern remains that the PCP care team will not have the ability to take on complex oncology patients and continue appropriate management. With the implementation of this and other tools, we are looking to better educate and prepare for this transition. With the increase of cancer patients and survivors, it remains difficult to manage current volumes of patients. Although the discussed changes have been helpful in optimizing our Survivorship program, it is a difficult task for PCPs to assume responsibility for the monitoring and surveillance of cancer patients. While we work to fill this gap with education and guidance, it would be helpful to increase Survivorship program staff to best serve our patients. There have been difficulties without an advanced practice provider following these patients for survivorship. The biggest difficulty has been that screening imaging cannot be easily ordered; the Survivorship RN navigator will communicate needs to the PCP team or past oncology team instead. At times, this has been frustrating to this patient population and has led to delays in management. The hope is that with the better collaboration between the Survivorship program and the PCP that there is better communication and follow-through to ensure that the patient is being appropriately monitored. To ensure responses from all survivorship patients, it would be helpful to offer the patient surveys through additional methods in case the patient does not utilize their EMR.
Conclusion
Patient navigators are responsible for addressing healthcare cancer disparities and work to improve overall quality of life for cancer survivors.5 Survivorship programs have been implemented as a strategy to improve care coordination and long-term follow-up care for survivors who have transitioned out of active cancer treatment.5 There are many survivorship care models that are coordinated and facilitated by different healthcare professionals. Our Survivorship program transitioned from being APN- to RN-driven, and, overall, this change has been well received. The changes implemented thus far have been shown to increase the number of patients being impacted by this program and to increase the collaboration between the oncology teams and the PCPs, ensuring that the needs of this patient population are more personalized and well met. There are continued opportunities to improve the relationship between the oncology teams and PCP care teams.
References
- Institute of Medicine. Implementing Cancer Survivorship Care Planning: Workshop Summary. The National Academies Press; 2007.
- National Cancer Institute. The Division of Cancer Control & Population Sciences. Office of Cancer Survivorship. 2022. https://cancercontrol.cancer.gov/ocs/statistics
- Flores T, Glaser KM, McDaniel D, et al. Building a comprehensive cancer survivorship program. ecancer. 2019.
- Kantsiper M, McDonald EL, Geller G, et al. Transitioning to breast cancer survivorship: perspectives of patients, cancer specialists, and primary care providers. J Gen Intern Med. 2009;24(suppl 2):S459-S466.
- Phillips S, Villalobos A, Pratt-Chapman M. Evaluating an online training course to develop and sustain cancer navigation and survivorship programs. Oncol Nurs Forum. 2019;46:E171-E179.