Background: Approximately one-half of adult cancer patients experience clinically significant psychological distress. Distress diminishes quality of life (QOL) and may interfere with patients’ treatment compliance and outcomes.
Objectives: To prospectively assess the effect of a navigation program on both distress and health-related QOL in a population of cancer patients.
Methods: Cancer patients who had navigators were evaluated at enrollment and again at 3, 6, 12, and 18 months. At each time point patients were administered the National Comprehensive Cancer Network Distress Thermometer (DT) and the Functional Assessment of Cancer Therapy – General (FACT-G).
Results: Of 297 evaluable patients enrolled between February 2012 and February 2015, 71% received chemotherapy, 8% radiotherapy, and 13% hormonal therapy. DT scores, FACT-G total scores, subscales physical well-being, functional well-being, and emotional well-being all significantly improved from 6 to 18 months after enrollment. Both high and low users of the program had improved DT scores, total FACT-G scores, and various FACT-G subscale scores. Patients expressed high satisfaction with navigation.
Discussion: This investigation found that distress and QOL improved over a period of 18 months while patients were in a navigation program after a diagnosis of cancer. DT and FACT-G scores improved whether patients were high or low users of the program. Lack of a control group makes definitive conclusions difficult.
Conclusion: This navigation program may have positively impacted both distress and QOL in this cohort of cancer patients during and after treatment over a period longer than previously reported.
Patient navigation is the process of providing individualized care to patients with the goal of improving a variety of healthcare measures: socioeconomic disparities in care, resource utilization, education, communication, coordination of services, patient adherence to therapy, quality of life (QOL), and ultimately, survival.1-5 The first patient navigation program was established in 1990 in Harlem, NY, to address a dramatic disparity in breast cancer mortality among minority women. The success of that program provided the impetus for the development of similar programs across the country and for federal support of patient navigation research.1
Despite the implementation of many patient navigation programs across the country, determining a program’s effectiveness has been challenging. Navigation programs are diverse in personnel and services.2-4 In 2008, the National Cancer Institute sponsored the formation of the Patient Navigation Research Program (PNRP) with the charge to design, implement, and evaluate a generalizable navigation program.5 The PNRP defined patient navigation as support and guidance offered to “vulnerable” persons with…a cancer diagnosis, with “the goal of overcoming barriers to timely, quality care.” Primary outcomes of the PNRP were time to diagnostic resolution, time to initiation of treatment, patient satisfaction with care, and cost-effectiveness. QOL was categorized under patient satisfaction outcomes.
Approximately one-half of adult cancer patients experience clinically significant psychological distress.6 Distress not only naturally diminishes QOL, it can also interfere with patients’ treatment compliance, thereby affecting treatment outcomes.7 Of the voluminous literature on patient navigation, relatively few studies report the effect of patient navigation on distress and QOL, and those studies show inconsistent results.7-10
Distress and QOL are considered important variables that a patient navigation program should positively impact.11 This study prospectively assessed the effect of our patient navigation program on both distress and health-related QOL in our population of cancer patients. We hypothesized that measurements of distress and QOL would improve with higher utilization of patient navigation based on the number of patient contacts with navigators and the number of support services used by patients.
Methods
Our navigation team includes 5 nurses and 2 nonclinical associates in a community teaching institution. This team assists in coordinating care for patients with all cancers. Nurse navigators are assigned to all breast cancer patients, and patients with all other cancers are identified for needing assistance by navigators reviewing pathology reports, attending hospital rounds, and responding to requests from physicians, social workers, and other cancer services staff who recognize a need for support. Nurse navigators educate patients about their cancers, treatment, and recovery; the team assists with difficulties in scheduling tests and directs patients to multiple support services within the cancer program, including an integrative medicine clinic, based on need. Patients meet with navigators based on individual needs and also have set follow-up calls with navigators that vary by cancer department.
Research staff identified patients for the study from navigator records. At the oncologists’ offices either research staff or a navigator obtained written consent and enrolled the patients. Eligibility criteria were diagnosis of cancer or recurrence within the prior 6 months, English-speaking, ≥18 years of age, and no obvious barriers to complete the 18-month process of surveys (eg, transportation difficulties, plans to move residence). Patients may have been using the navigation program prior to enrollment in the study. This study was approved by the OhioHealth Corporation Institutional Review Board 1, #1066720.
At enrollment to the study, the research staff collected demographic and personal health information, and baseline data on the number of contacts with navigators and utilization of cancer support services since the diagnosis of cancer and prior to enrollment.
The research staff administered the Functional Assessment of Cancer Therapy – General (FACT-G) and the National Comprehensive Cancer Network (NCCN) Distress Thermometer (DT) to patients at enrollment and again at 3, 6, 12, and 18 months after enrollment. They assisted the patients in completing both instruments either in person, by phone, or by mail. At these same time points, they also surveyed the patients either in person or by phone to obtain information on the number of contacts with their navigators and the number of cancer support services and resources used during the prior time interval. Patients may not have answered a survey at a particular time point, but they were not considered dropouts unless they did not complete the final (18-month) survey. At the end of the study they were administered a brief satisfaction survey about the navigation program.
To capture an overall assessment of the navigation program, the number of navigator contacts with patients was combined with the number of support services utilized by patients. Primary outcomes were QOL and patient distress. The FACT-G (version 4) measured QOL, and the DT measured distress.
A clinically significant difference in FACT-G total scores is about 5 points, and 1 to 2 points in the FACT-G subscales.12 The standard deviation of total scores in various patient subgroups ranges from about 15 to 20.12 Therefore, to detect a difference of 5 points in mean scores, with an assumed standard deviation of 17.5, 80% power, a Type I error rate of 5%, and a 10% dropout rate, the minimum sample size required was 286 patients. However, we anticipated unequal sample allocations and/or multiple categories for many of our subgroup comparisons. Therefore, we increased our total sample size to 320 patients. A sample size of 320 also provides greater than 99% power to detect a mean difference of 1.5 in DT scores over time. A clinically meaningful change score for the DT was not identified in the literature.
Within-group changes from baseline were analyzed with repeated measures analysis of variance models. Potential correlations between the DT scale and the FACT-G scores were assessed at each time point using the Spearman correlation method, with a coefficient of 0.5 to 0.7 in absolute value indicating a moderate to strong relationship. Baseline and demographic characteristics were assessed for relation to QOL changes using multivariable analysis of variance methods. All inference testing was completed with a 2-tailed alpha level of 5%. P values ≤.05 were considered statistically significant, and all results were also considered for clinical significance as mentioned above. All calculations used patient-reported outcomes (PROs). Statistical Analysis Software V9.4 was the package for analysis.
Results
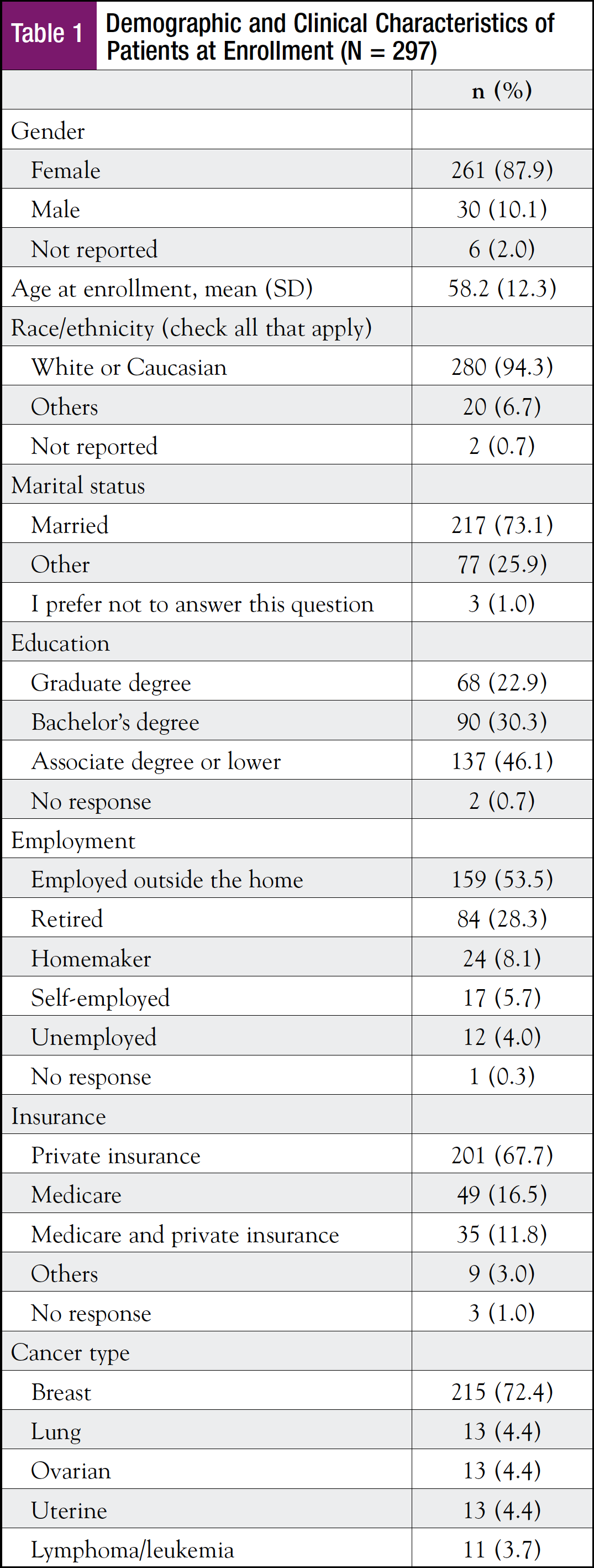
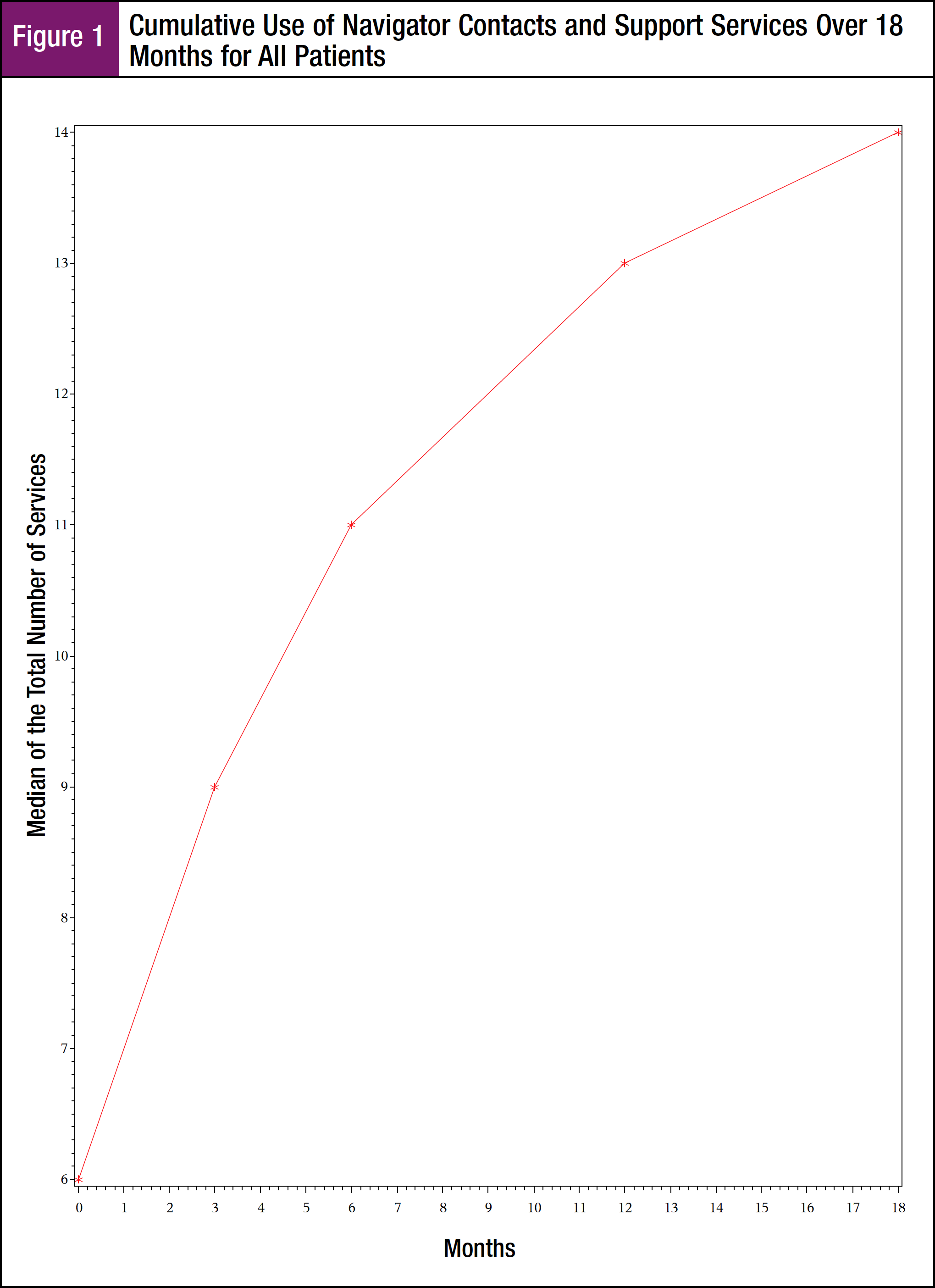
Between February 2012 and February 2015, the study enrolled and consented 320 patients, of whom 314 were eligible due to completing at least 1 time point assessment. Seventeen patients were removed due to enrolling more than 180 days after their diagnoses of cancer, leaving 297 evaluable patients. Table 1 details demographics and clinical characteristics. The high proportion of breast cancer patients was due to the breast cancer program having an advanced navigator program established several years before other cancer site programs. Only 2 patients were enrolled after a diagnosis of recurrent cancer.
Seventy-one percent of patients were receiving chemotherapy at baseline evaluation. Of these, approximately one-half had completed 2 cycles; another 30% had completed either their third or fourth cycle.
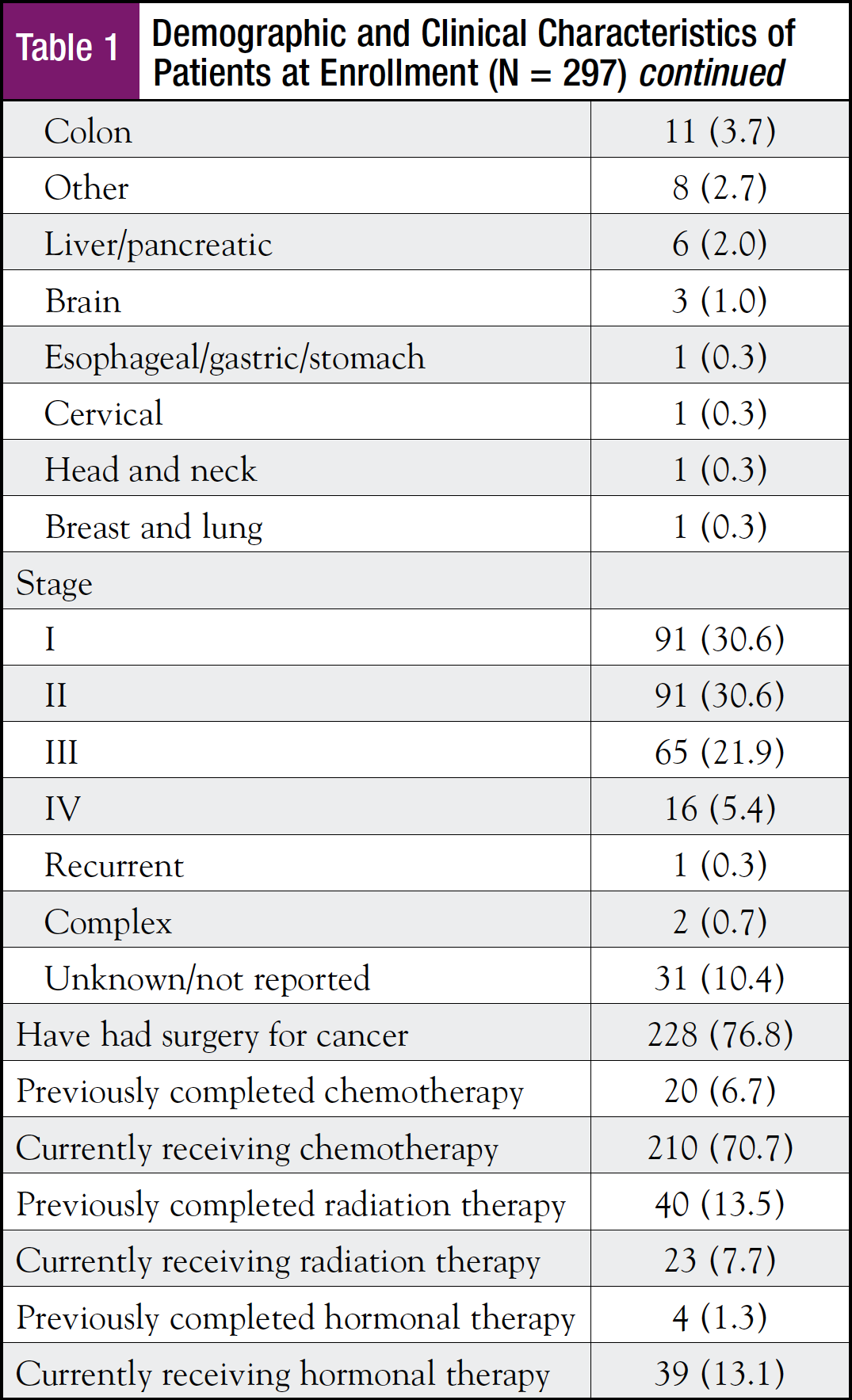
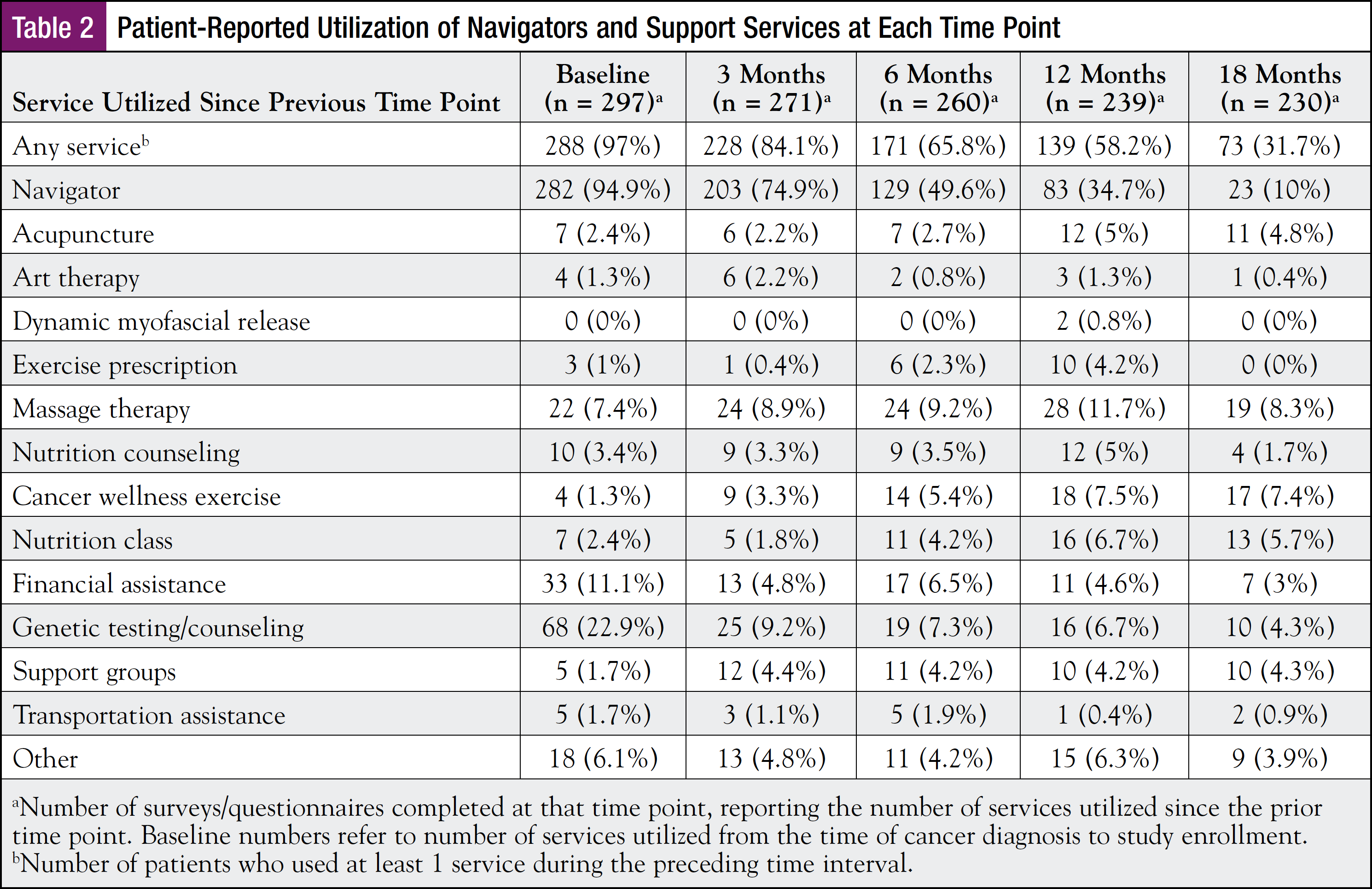
Table 2 shows the number of patients using the navigators and various support services at each time point. Some of these services were interpreted as complementary integrative medicine (CIM)—exercise, art therapy, acupuncture, nutrition counseling, and massage. Figure 1 shows the cumulative utilization of navigators and support services over 18 months.
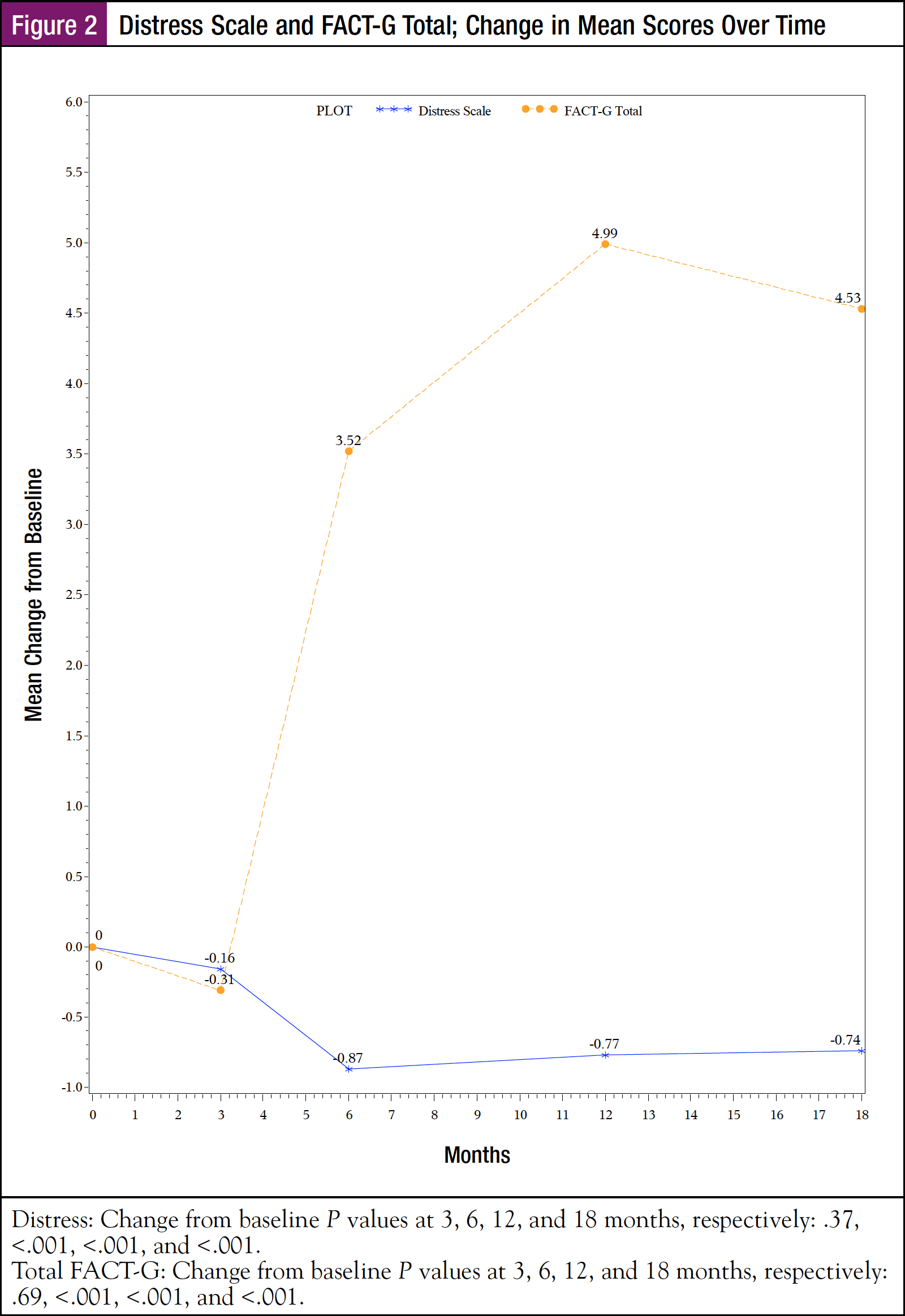
DT scores significantly improved from 6 to 18 months (Figure 2). The DT records distress in problematic domains: practical, family, emotional, spiritual, physical, and “other.” At baseline, patients reported the most problems with nervousness, worry, fatigue, and sleep (41%-67%). These distresses remained the most prevalent across all time points, but the proportions declined (21%-39%) by 18 months. Approximately 30% of patients recorded problems with memory or concentration at baseline and all time points.
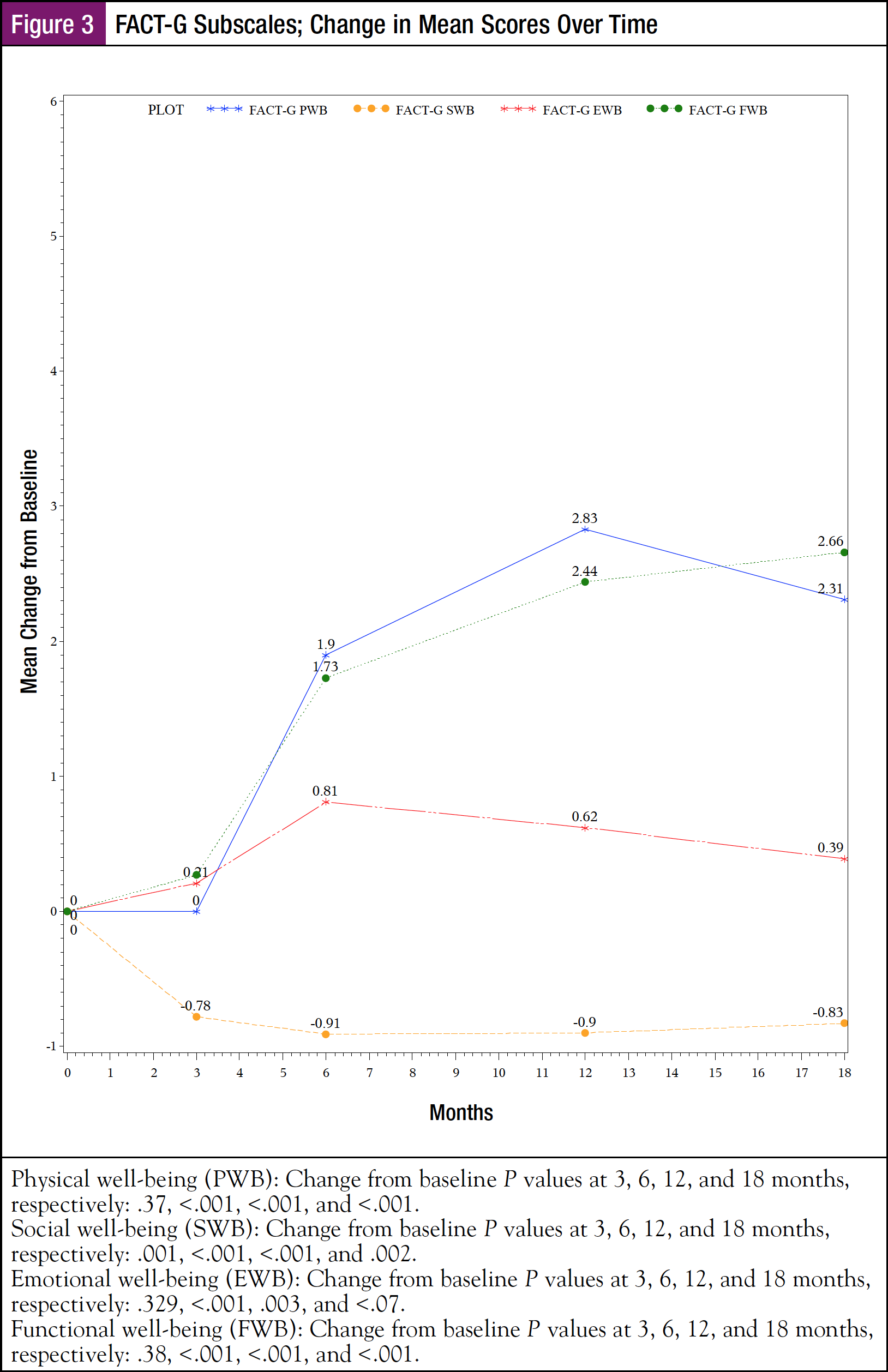
Both FACT-G total scores and FACT-G subscale scores of physical well-being (PWB), emotional well-being (EWB), and functional well-being (FWB) significantly improved from 6 months to 18 months after enrollment (Figure 2 and Figure 3). Using a 5-point change for total FACT-G and a 1-point change for subscales, the improvement was also clinically significant for total FACT-G at 12 months (nearly significant at 18 months) and for PWB and FWB at 3, 6, and 12 months. Social well-being (SWB) significantly declined over all time points; however, the decline was not clinically significant.
DT scores were moderately to highly related to total FACT-G scores across all time points (Spearman coefficients 0.61-0.68), moderately related to subscales PWB, EWB, and FWB (coefficients 0.42-0.62), and weakly related to SWB (coefficients 0.28-0.42).
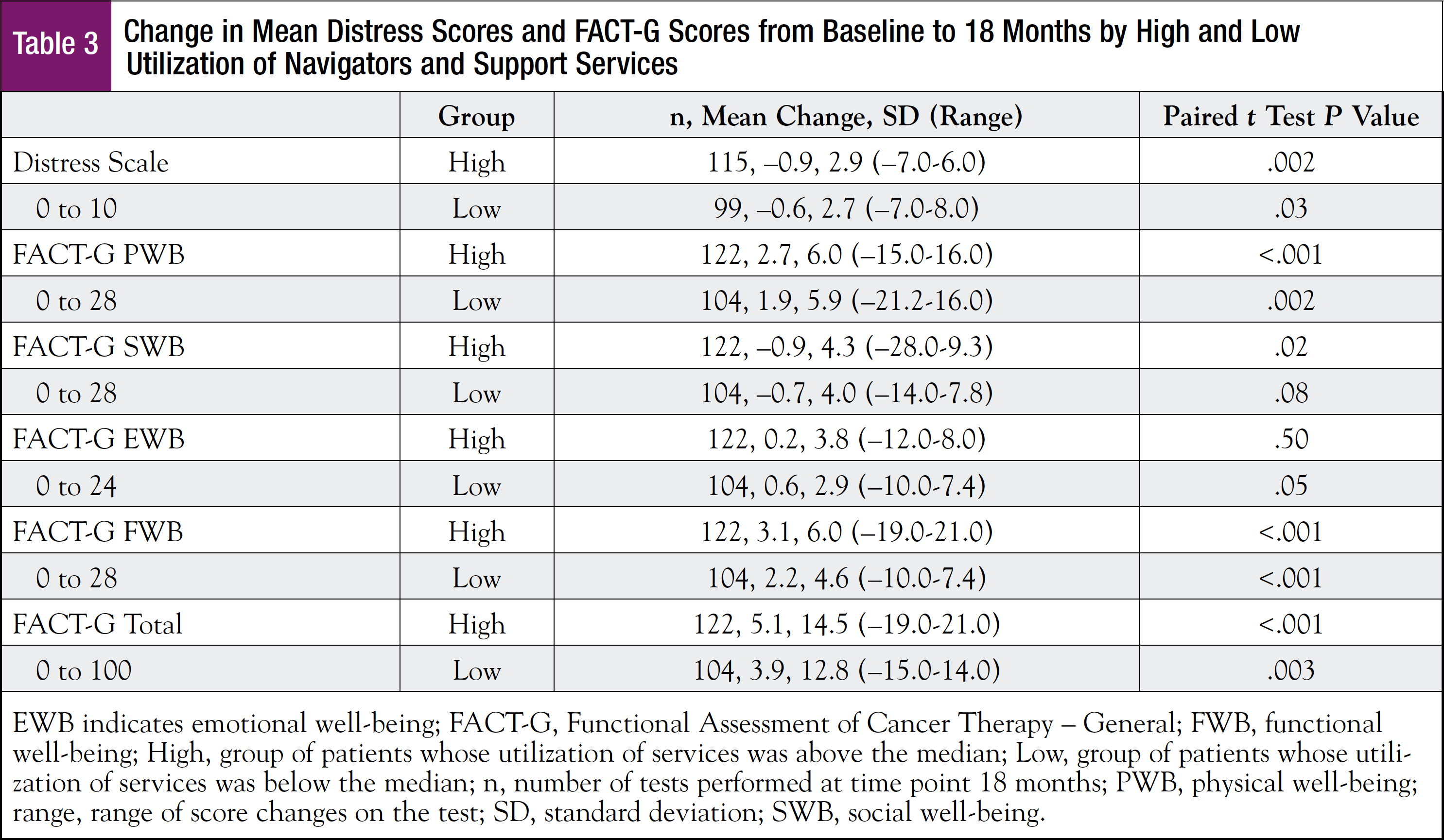
The cumulative utilization of the navigation program (navigator contacts plus support services) over the study period was not significantly associated with either DT scores or FACT-G scores (Spearman coefficients –0.01-0.15 at all time points). To look at utilization from a different perspective, the cohort was divided into high and low users of the navigation program, a division created by separating patients above and below the median number of patients’ total usage. Across all time points both high and low users had statistically significant improvement in DT scores, total FACT-G scores, and subscales PWB and FWB (Table 3). When using the clinically meaningful mean score changes, high users had a clinically significant improvement in total FACT-G, PWB, and FWB; low users had clinically significant improvement in PWB and FWB. The range of time between cancer diagnosis and enrollment was considerable. Analysis showed no correlation between this variable and utilization of the navigation program (data not shown).
Overall, patients reported satisfaction with patient navigation. After the 18-month time point, 240 patients answered 1 or more questions on the Patient Satisfaction Survey, which used a Likert scale (1 = not at all/least, 5 = most/greatest). The most significant question was “Based on your experience with patient navigation, would you recommend a navigator to a patient diagnosed with cancer?” The mean response was 4.6 (SD, 0.7; median, 5.0). The most helpful resources were phone calls with a navigator (76%) and face-to-face meetings with navigators (50%).
Discussion
This investigation found that distress (NCCN DT) and QOL (FACT-G) improved over a period of 18 months while patients were in a navigation program after a diagnosis of cancer. DT and FACT-G scores improved for patients whether they were high or low users of the program. However, patients’ cumulative utilization of both the navigators and the support services of the program was not significantly associated with changes in either distress scores or QOL. Although the results do not support this study’s initial hypothesis that distress and QOL would correlate with the extent of utilization of the navigation program, the data suggest that the navigation program may have positively impacted distress and QOL by patients using the level of services they needed.
PROs and data were used for statistical analysis. Investigators have determined that PROs are suitable for evaluating patient navigation.11 In addition, these same investigators contend that assessment of QOL is among the most meaningful of PRO measures.
The difference between statistical and clinical significance is important when evaluating QOL. Prior work with FACT-G has indicated that a mean change of 5 to 7 points in total FACT-G and 1 to 2 points in subscales are clinically significant based on Global Rating of Change data.12 Accordingly, our data showing statistically significant improvement in total FACT-G and subscales PWB and FWB also have clinically meaningful significance. EWB and SWB changes were not clinically meaningful, although statistically significant in some subgroups. Perhaps navigation did not meet the social and emotional needs of this cohort. Another possibility is that these FACT-G subscales may not be the best instruments to measure changes in these domains in this particular population.
Published studies also using the FACT-G instrument have indicated that chemotherapy is associated with a decline in QOL.13,14 Additional studies using a variety of QOL instruments have shown that QOL declines after a cancer diagnosis and during its treatment.15-19 The recovery time for QOL to return to baseline is variable, from a few months to at least 2 years after therapy.18,20 Ninety percent of our cohort was undergoing treatment at enrollment, mostly chemotherapy (71%), but also radiotherapy and hormonal therapy. Chemotherapy regimens are typically administered over 6 to 8 months. One study of gynecologic cancer patients discovered that although QOL improved after treatment, it remained stable from 6 to 12 months after chemotherapy.21 In our study, both distress and QOL significantly improved at 6 months after enrollment at a time when many of the patients may just have been completing chemotherapy, and it continued to improve over the next 12 months. This pattern indicates a possible deviation from what normally would be expected for those domains. Thus, perhaps utilization of the navigation program can account for this deviation, namely, amelioration of a decline, or even improvement, in distress and QOL. Of course, this improvement in distress and QOL may have been the normal course for this cohort. The number of confounding variables and the lack of a control group make a definitive conclusion difficult.
Our study adds to the conflicting reports on the relationship between navigation and distress and QOL. One retrospective review,7 a case-control study,9 and a randomized controlled trial8 all found a positive association between navigation and distress, or QOL, or anxiety. On the contrary, 2 randomized controlled trials found no impact of navigation on distress or QOL.10,22 These trials followed patients for 3 to 6 months. Even the PNRP stipulated the timing of metrics to be within 3 months of initiation of cancer treatment. A 3- to 6-month interval may not be sufficient time to evaluate the efficacy of patient navigation intervention. Our study tracked QOL and distress over 18 months, an additional 12 months; 47% of patients (139 of 297) continued to use navigation services for 6 of those months, and 25% (73 of 297) for the last 6 months (Table 2). This additional surveillance time could be considered a strength of this investigation.
Our goal was to assess the impact of the entire navigation program, which included support services. Up to 85% of patients initially diagnosed with cancer use CIM.23 The broad use of such support services is a major obstacle to enrolling control groups in QOL studies. Some research suggests that CIM can improve QOL in cancer patients.24,25 A meta-analysis of 34 randomized controlled trials with 3010 cancer patients “showed clearly superior efficacy of CIM in improving health-related QOL” without evidence of publication bias.25 That study found that the most efficacious services were exercise, mindfulness, acupuncture, and massage, several of which were accessible to our patients. Because CIM was a significant portion of the services in the navigation program that was associated with improved distress and QOL, results of the current study may support prior work demonstrating the positive effect of CIM on health-related QOL.
One interesting result was the moderate-to-strong correlation between the DT and FACT-G scores. Other investigators have reported similar findings.26,27 Using the DT and its problem list may present a more efficient method of assessing patient QOL than completing the FACT-G, not only for the patient but also for calculating scores.
A clear limitation of this study is the lack of a control population. We agree with other researchers who noted the practical and ethical difficulties in randomizing such studies that would thereby deny navigation services to the control group.7,10 In addition, many of our patients may seek navigation services without the direction of a navigator; therefore, identifying a control group who did not, or would not, seek support services would be improbable. Prior studies have had difficulty defining comparable control groups.28,29
Another limitation in our work was determining the accuracy of patient-reported utilization of the navigation program. Relying on patient recall of events in the prior 3 months is suboptimal, and we had no method to check all utilization, so numbers could be either overreported or underreported. Nonetheless, the accuracy of patient recall is less important when considering our finding that both high and low utilization of the program may have positively impacted distress and QOL.
One additional limitation is the dropout rate. Our calculation for enrollment assumed a dropout rate of 10%. The implied dropout rate in this study was 67 (22%; 297 enrolled patients minus 230 completing the final surveys). This implied rate is greater than 10%, so the study may have been underpowered for any associations that did not have statistical significance; however, that occurred only in some of the FACT-G subdomains. The dropout rate could adversely affect the significant change in scores from baseline to 18 months if patients dropped out due to deteriorating status. However, the range of change scores in Table 3 indicates that some patients remained in the study despite increasing distress and diminishing QOL. Other reasons for dropping out would not likely affect the mean change (eg, survey fatigue, or loss of interest due to a prolonged time interval from diagnosis and treatment).
Even though navigation may not be directly associated with improving distress and QOL, patients derive satisfaction from a navigation program, as our study and others have shown.7-9,22 Simply inquiring about distress can increase satisfaction.7 The fact that a large proportion of patients continued to use the navigation program for 18 months indicates their satisfaction and the importance of the program to their overall care. Whether patient satisfaction by itself can justify the expense of a navigation program is a question for each individual institution.
Notably, the emphasis of this study was on distress and QOL, with no intention of analyzing any of the other outcomes listed by the PNRP. Those are extremely important for considering the merits and costs of a navigation program. Our experience with the impact of a navigation program, which incorporates support services including CIM, on distress and QOL warrants further support and research of the navigation program.
References
- Freeman HP, Muth BJ, Kerner JF. Expanding access to cancer screening and clinical follow-up among the medically underserved. Cancer Pract. 1995;3:19-30.
- Robinson-White S, Conroy B, Slavish KH, Rosenzweig M. Patient navigation in breast cancer: a systematic review. Cancer Nurs. 2010;33:127-140.
- Wells KJ, Battaglia TA, Dudley DJ, et al. Patient navigation: state of the art or is it science? Cancer. 2008;113:1999-2010.
- Paskett ED, Harrop JP, Wells KJ. Patient navigation: an update on the state of the science. CA Cancer J Clin. 2011;61:237-249.
- Freund KM, Battaglia TA, Calhoun E, et al. National Cancer Institute Patient Navigation Research Program: methods, protocol, and measures. Cancer. 2008;113: 3391-3399.
- Jacobsen PB, Ransom S. Implementation of NCCN distress management guidelines by member institutions. J Natl Compr Canc Netw. 2007;5:99-103.
- Swanson J, Koch L. The role of the oncology nurse navigator in distress management of adult inpatients with cancer: a retrospective study. Oncol Nurs Forum. 2010;37:69-76.
- Ferrante JM, Chen PH, Kim S. The effect of patient navigation on time to diagnosis, anxiety, and satisfaction in urban minority women with abnormal mammograms: a randomized controlled trial. J Urban Health. 2008;85:114-124.
- Fillion L, de Serres M, Cook S, et al. Professional patient navigation in head and neck cancer. Semin Oncol Nurs. 2009;25:212-221.
- Skrutkowski M, Saucier A, Eades M, et al. Impact of a pivot nurse in oncology on patients with lung or breast cancer: symptom distress, fatigue, quality of life, and use of healthcare resources. Oncol Nurs Forum. 2008;35:948-954.
- Fiscella K, Ransom S, Jean-Pierre P, et al. Patient-reported outcome measures suitable to assessment of patient navigation. Cancer. 2011;117(15 Suppl):3603-3617.
- Cella D, Hahn EA, Dineen K. Meaningful change in cancer-specific quality of life scores: differences between improvement and worsening. Qual Life Res. 2002;11:207-221.
- Rithirangsriroj K, Manchana T, Akkayagorn L. Efficacy of acupuncture in prevention of delayed chemotherapy induced nausea and vomiting in gynecologic cancer patients. Gynecol Oncol. 2015;136:82-86.
- Sanford SD, Wagner LI, Beaumont JL, et al. Longitudinal prospective assessment of sleep quality: before, during, and after adjuvant chemotherapy for breast cancer. Support Care Cancer. 2013;21:959-967.
- Hall E, Cameron D, Waters R, et al. Comparison of patient reported quality of life and impact of treatment side effects experienced with a taxane-containing regimen and standard anthracycline based chemotherapy for early breast cancer: 6 year results from the UK TACT trial (CRUK/01/001). Eur J Cancer. 2014;50:2375-2389.
- Leinert E, Singer S, Janni W, et al. The impact of age on quality of life in breast cancer patients receiving adjuvant chemotherapy: a comparative analysis from the prospective multicenter randomized ADEBAR trial. Clin Breast Cancer. 2017;17:100-106.
- Browall M, Ahlberg K, Karlsson P, et al. Health-related quality of life during adjuvant treatment for breast cancer among postmenopausal women. Eur J Oncol Nurs. 2008;12:180-189.
- Pearman T. Quality of life and psychosocial adjustment in gynecologic cancer survivors. Health Qual Life Outcomes. 2003;1:33.
- Bonomi P, Kim K, Fairclough D, et al. Comparison of survival and quality of life in advanced non-small-cell lung cancer patients treated with two dose levels of paclitaxel combined with cisplatin versus etoposide with cisplatin: results of an Eastern Cooperative Oncology Group trial. J Clin Oncol. 2000;18:623-631.
- Greimel E, Thiel I, Peintinger F, et al. Prospective assessment of quality of life of female cancer patients. Gynecol Oncol. 2002;85:140-147.
- Chan YM, Ngan HY, Li BY, et al. A longitudinal study on quality of life after gynecologic cancer treatment. Gynecol Oncol. 2001;83:10-19.
- Fiscella K, Whitley E, Hendren S, et al. Patient navigation for breast and colorectal cancer treatment: a randomized trial. Cancer Epidemiol Biomarkers Prev. 2012;21:1673-1681.
- Judson PL, Abdallah R, Xiong Y, et al. Complementary and alternative medicine use in individuals presenting for care at a comprehensive cancer center. Integr Cancer Ther. 2017;16:96-103.
- Domnick M, Domnick M, Wiebelitz KR, Beer AM. Evaluation of the effectiveness of a multimodal complementary medicine program for improving the quality of life of cancer patients during adjuvant radiotherapy and/or chemotherapy or outpatient aftercare. Oncology. 2017;93:83-91.
- Lin WF, Zhong MF, Zhou QH, et al. Efficacy of complementary and integrative medicine on health-related quality of life in cancer patients: a systematic review and meta-analysis. Cancer Manag Res. 2019;11:6663-6680.
- Wang X, Lv Y, Li W, et al. Correlation between psychosocial distress and quality of life in patients with nasopharyngeal carcinoma following radiotherapy. J Oncol. 2018;2018:3625302.
- Head BA, Schapmire TJ, Keeney CE, et al. Use of the Distress Thermometer to discern clinically relevant quality of life differences in women with breast cancer. Qual Life Res. 2012;21:215-223.
- Lee T, Ko I, Lee I, et al. Effects of nurse navigators on health outcomes of cancer patients. Cancer Nurs. 2011;34:376-384.
- Wagner EH, Ludman EJ, Aiello Bowles EJ, et al. Nurse navigators in early cancer care: a randomized, controlled trial. J Clin Oncol. 2014;32:12-18.