Abstract: Modern medicine has long been focused on the hard science that drives change through numbers-based analysis and data-driven metrics. This has certainly allowed for significant progress to be made in healthcare, resulting in better treatment options, better patient safety, and better outcomes. Sometimes it seems that soft science principles, those ideas and data based on human behavior, are considered merely optional. A review of relevant studies shows many of the ways this omission has directly contributed to low satisfaction rates for both patients and providers. Soft skills can still be science and data based. This paper includes patient comments and introduces the concept of compassion science, which uses data collected within the fields of trauma and cognitive science to improve care and outcomes for oncology patients, increase trust and satisfaction levels for both patients and providers, and decrease the overall cost of care.
Data-Driven Practices
Healthcare is well known for its adherence to data-driven practices. With the rapid advances in medicine and practitioners’ understanding of disease processes, this adherence is necessary to keep up with current treatment and safety recommendations. In 1950, within the field of oncology, it had taken approximately 50 years for cancer knowledge to double. By 1980 this time had decreased to only 3.5 years. Today cancer knowledge doubles approximately every 73 days.1
Healthcare is known for its adherence to data-driven practices. With the rapid advances in medicine and practitioners’ understanding of disease processes, this adherence is necessary to keep up with treatment and safety recommendations.
Healthcare’s focus on research and data-driven metrics has allowed providers to achieve better outcomes with more customized treatments and safer, more effective practices. However, we in healthcare still face significant challenges.
Oncology knowledge may be doubling rapidly, but the World Health Organization estimates that the number of cancer cases is expected to increase by almost 50% between 2020 and 2040.1 Fortunately, cancer patients have access to better treatments and medications and are living longer, but associated healthcare costs are climbing; the United States currently spends more than $200 billion annually on treating cancer.1 Cancer has also been named the disease most feared by patients,2 and recent reports by the Beryl Institute3 show the lowest trust level in US healthcare since data started being collected. Here we face a problem—with a wealth of knowledge at our fingertips cancer patients have a more optimistic prognosis than at any other time in history, yet the fear and distrust surrounding this disease and its care are higher than ever. Within that fear and distrust lie concurrent issues, including poor compliance to treatments, high rates of depression and anxiety, and 75% of patients leaving their doctor’s office feeling confused by information they were given.4
What are we missing? Many answers can be found in data from trauma and cognitive science. These areas of study provide the opportunity to focus not only on information but also on how that information is presented and if it’s being received in a way that meets the needs of patients.
Trauma-Informed Care
The Substance Abuse and Mental Health Services Administration described trauma-informed care:
“A program, organization, or system that is trauma-informed realizes the widespread impact of trauma and understands potential paths for recovery; recognizes the signs and symptoms of trauma in clients, families, staff, and others involved with the system; and responds by fully integrating knowledge about trauma into policies, procedures, and practices, and seeks to actively resist re-traumatization.”5
In the field of oncology, understanding trauma starts with the knowledge that trauma can occur for all parties involved in high-stress situations; this includes the patient, their support people, and the medical staff. Trauma overwhelms coping mechanisms, frequently requiring outside intervention in order to recover in a timely and complete way. A patient’s cancer diagnosis can easily overwhelm their coping mechanisms, and providing support can overwhelm caregivers as well.
Using the study of trauma to improve cancer care means that healthcare providers recognize that many patients are in a traumatized or overwhelmed state after receiving a cancer diagnosis, and that when people operate from this highly stressed state they do not process information well. In what has often been referred to as an “amygdala hijack” (a term coined by psychologist Daniel Goleman), the body’s response to a threatening situation results in the brain going into survival mode, which is a chemical process as well as a mental process.6
In most cases, stress and trauma change the way that people take in, process, and retain information. Take Sarah’s experience as an example. She recounted that when she received her cancer diagnosis, “All I heard were the words ‘you have cancer,’ and the rest of the words were like listening to the adults in a Charlie Brown special—it was just mumbled background noise.” Sarah went on to say that even though she didn’t remember the words, she remembered the art that was on the doctor’s desk and the smell of the hallway. Sarah’s brain was attempting to assess and process a threat, leaving no room for the complex information she was being given about her diagnosis. Maslow’s hierarchy of needs is well represented here in that, if safety is not established first, more complex needs (for information, for autonomy, and for improved control) cannot be effectively processed or addressed.7
And what about the care team repeatedly giving devastating news to their patients? The field of psychology acknowledges that medical personnel can be at a high risk of suffering from second-hand trauma, and certainly this is a contributor to clinical staff stress and turnover.6 A provider’s response to a patient or to the patient’s situation may lead all parties in a conversation to experience a heightened level of stress or trauma. Trauma science can assist providers to deliver better care. The first step is ensuring that staff have adequate training to identify, address, and de-escalate stress responses in their patients and themselves. The second is recognizing how to target communication in a trauma-informed manner, using the considerations of cognitive science and processing.
Cognitive Science and Learning
As in Sarah’s case, physicians frequently give a devastating diagnosis to a patient and, by necessity, start giving information and asking for decisions before the patient has been able to recover from their brain’s shift into threat response. The patient is still in that survival mode, which is the worst possible state in which to process complex information.6-8 If care providers can find ways to offer reassurance, a sense of safety, and a sense of being compassionately cared for, the patient may experience releases of endorphins and dopamine—chemicals that help the brain to reengage with the prefrontal cortex and its ability to perform higher-level thinking. These same chemicals also help to encode memory more deeply.8
Training staff in how trauma and cognitive principles affect learning can be an incredibly effective way to teach communication tactics that are trauma-informed and hence enable staff to provide information that is absorbed more completely by the patient.
Information is only helpful if the person receiving it understands it. Or, to borrow the words of George Bernard Shaw, “The single biggest problem with communication is the illusion that it has taken place.” Healthcare professionals spend years of dedicated study ensuring that the information they give is current and valuable. Why then is the opportunity being missed—by not taking minutes to hours using scientifically proven methods—to ensure that the information is delivered effectively? Understanding the fears and cognitive biases of patient populations can prepare staff to mitigate those factors to make patients more active care partners and improve compliance with and tolerance of care regimens.9,10
Oncology care providers can better address patient concerns if they understand the cognitive science behind how the brain works. As an example of these concerns, alopecia is recognized as one of the most feared side effects of chemotherapy for women. Carrie, a young woman saying goodbye to her mother in the ICU, stated her mother had refused chemotherapy for her—now advanced—cancer because she feared losing her hair, which was the first thing her husband noticed about her when they met. Her hair was also a symbol of her relationship with children, as they would often play with her hair when cuddling. Carrie was now questioning if help with this identity threat might have given her mother a better chance at survival. Hair loss can be especially threatening to self-identity, and this is even more so in certain cultures that specifically identify hair as a symbol of power or sexuality. Up to 8% of women may be refusing recommended chemotherapy treatment because of this fear.11,12 The risk is more severe for already vulnerable populations, such as those of African American heritage. Thousands of women annually may be refusing needed care due to unaddressed fear or identity threat (Figure 1).

The fear of hair loss is only one example of identity threat, which is the actual or perceived loss of the things human beings use to define themselves and their role in society. This threat can lead to involuntary psychological and physiological processes that when experienced repeatedly can have detrimental consequences for health.13 Evidence shows that people respond to perceived or expected judgments with the same biochemical and behavioral changes that occur with actual judgments.14,15 Identity threat can present a significant barrier to patient recovery and is applicable to most people who are suffering from a complex disease. Their self-image can be affected, but so can their physical abilities, which contribute to how they may define themselves as a person within their family or work structure. Compassionate care mandates that whenever possible healthcare teams work to identify and address these psychosocial threats and repercussions. Simply identifying a patient’s greatest perceived threat provides an opportunity for discussion and intervention. That intervention may be a simple conversation, an educational resource, or a referral to a support group or counselor.
Identity threat can also be mitigated by creating a sense of belonging within a group. This may mean a specifically appointed support group of others who are on a similar health journey but could represent any transition to a supportive new group (such as a church group or an art therapy class). An important consideration in helping patients to identify a new group is the cognitive science principle of availability heuristic: people estimate their own success or failure based on the immediate examples their brain gives for comparative people or circumstances. Therefore, ensuring that positive stories are part of any diagnosis-specific support group is paramount. After being newly diagnosed with breast cancer, Amanda said, “I wasn’t able to picture myself on the other side of this disease until I saw photos and stories of people who had made it through this. Seeing them still filled with life and hope gave me the ability to see myself there too.”
Although cognitive science principles offer an abundance of supportive information, one other factor is crucial regarding information presented to people with stressed or traumatized mindsets. The lowest retention rate human beings have for information is words that they hear8 (Figure 2). Yet often this is the way healthcare providers impart the most critical information to patients. If the recipient of information has just been thrust into trauma-processing mode, the retention rate is lower still.7 Almost everyone in medicine has had the experience of a patient returning who did not effectively process or retain the information that was given to them at a prior visit.
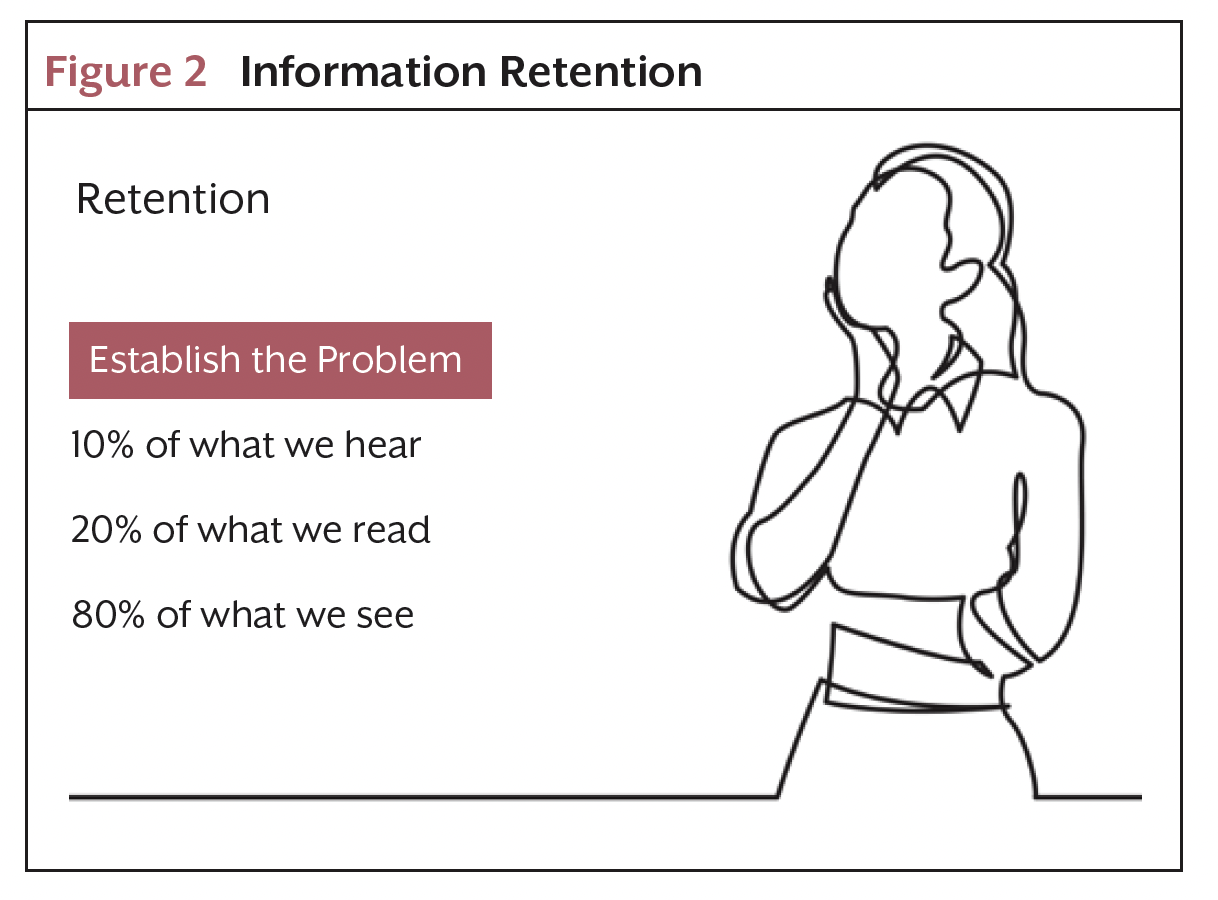
The tools used least in healthcare are actually the ones that are most effective. Picture superiority effect (PSE) tells us that our brains are far better at using information that contains visuals. “Human PSE is truly Olympian…tests performed years ago showed that people could remember 2,500 pictures with at least 90 percent accuracy several days post-exposure, even though the subjects saw each picture for about 10 seconds.”8 Add to this the modality principle, which packages narrative together with imagery, and information processing and retention for patients can improve from less than 10% with words alone to between 80% and 90%. This is because the brain is using multiple areas to both process and encode this multimodal input.8
One example of cognitive and trauma science principles being used to create an educational resource occurred among patients with breast cancer. A group of medical caregivers associated with the Asante and Providence health systems worked with a team of patients to determine the fears and threats that breast cancer patients identified as interfering with or slowing their recovery. Fifty patients gave narrative-based responses to the medical and support information that had been presented to them. They identified information that was effective and met their needs as well as information that missed that mark and was either not remembered or remembered as having different content or messaging than that which was intended.16
Using the principles of trauma-informed care and cognitive learning, the group created a new resource by collecting the survey data and putting the information they wanted to present through a trauma-informed, multimodal presentation focus. The resultant resource book16 leaned heavily on narrative teaching accompanied by visuals that provided information in a realistic yet simultaneously uplifting and hopeful manner. The cognitive principle of availability heuristic gave patient readers a selection of emotionally engaging success stories for them to compare with their own experience. PSE presented therapy and recovery strategies in visual format whenever possible (1 photo shows a patient engaged in fly fishing to reference the Casting for Recovery program, another shows a patient engaged in art therapy).
The story narratives that accompanied the photos allowed the team to present other recovery strategies that used complex science, such as internal scripting through the principles of neuroplasticity. Patients could use these strategies to increase their own agency and improve their recovery progress. The book is an example of what a resource based on the science of compassion can look like: heavy visuals, accompanied by narrative teaching, whose presentation format addresses identity threat concerns and leverages availability heuristic through the sharing of success stories.
Most importantly, feedback from patients who had used the resource indicated they were often able to process information that assisted with decision-making and recovery sooner and more completely.16
Pathophysiological Responses to Stress
Multiple categories of psychological and physical consequences have been associated with unaddressed stress and trauma among oncology patients. The following issues are reminders as to why both the information we present and the way that we present it matter so much.
Mental Health Consequences
Cancer patients have an increased risk of depression and anxiety (nearly twice that of comparative control populations), and a 50% increased risk of substance abuse.17 Oftentimes a perceived threat of judgment from others will result in withdrawal from social situations and intimacy.18 Both unaddressed identity threat and depression have been associated with poor quality of life as well as with chemical fallouts that create physical compromises to patients.
Physical Consequences
Increased activation of the hypothalamic-pituitary-adrenal (HPA) axis has been associated with depression, stress, and identity threat. Activation of the HPA axis can cause chronic inflammation associated with increased proinflammatory cytokines and increased C-reactive protein, which can contribute to decreased immune function and increased symptoms (including decreased tolerance of therapies).18-20 Chronic inflammation contributes to increased allostatic load, which also brings numerous health risks.15
Decisional Consequences
Fighting against identity threat can bring about cognitive fatigue resulting in poorer executive functioning (decreased ability to persevere, to make decisions, to maintain optimism). Perceived threats to a patient’s identity can also directly affect decision-making and participation in care planning.15
In the United States, the cost of treating an oncology patient with depression is twice that of treating a patient without depression: $235,337 as opposed to $110,650. The cost of replacing staff that have burned out can be in the billions.
If these issues required complex care interventions that the medical system would struggle to meet, they would present a much greater challenge. But simple measures, utilizing compassion-driven science, do make a difference.
Conclusion: Results of Using Compassion-Driven Science
Where to begin? If fields of study have shown that cancer patients are suffering moderate to high anxiety and depression,14,20 then simply recognizing some of the up to 80% of psychological and psychiatric morbidity that goes unrecognized and untreated would be a great start.20 The science of compassion begins with recognizing distress both above and below the surface of the patient’s presentation. Compassionate inquiry means healthcare providers need to ask more questions up front about what threats are most concerning to patients. In this way, providers can often address depression, anxiety, and disconnection prior to their sometimes catastrophic cascade of increased risk factors. When caregivers reach to address those threats, intentionally using language that is trauma-informed during communication and outreach is the next great step.
Healthcare professionals should deliver trauma-informed education and support by:
- Considering and addressing patients’ perception-based stress processing (use visuals and other multimodal methods)
- Providing simple, bite-sized information that patients can process easily even through mental fog
- Using repetition and reflection-based questions to verify understanding
- Connecting success stories from other patients experiencing similar disease trajectories
- Identifying and addressing patient-specific fears
- Including resources to address grief responses
- Providing access to information for both the patient and their support network
Quality of life is a great reason to be concerned about this issue, as is optimizing the potential for quality care and positive patient outcomes, but keeping costs down and ensuring high patient satisfaction scores and engagement are also positive results of these interventions.9,10
The main effects of poor communication in healthcare are a reduction in the quality of care, poor patient outcomes, waste of resources, and high healthcare costs.21 Communication failures often have a negative effect on patient and staff satisfaction.
Effective communication will:
- Improve quality of care and patient outcomes
- Enhance the patient experience
- Improve patient satisfaction scores
- Reduce the cost of healthcare
- Reduce stress for clinicians and prevent burnout
In the United States, the cost of treating an oncology patient with depression is twice that of treating a patient without depression: $235,337 as opposed to $110,650.22 The cost of replacing staff that have burned out can be in the billions. And additional billions are also lost on the costs of patient deaths and lawsuits that have resulted from poor communication. These costs provide fiscal and quality-focused motivation for seizing a science-based opportunity to improve communication.
Key headlines from consumer reports show that “listen to you” and “communicate clearly in a way you can understand” remain priority items for patients.3 Patients who feel that their care teams listened to their concerns and communicated effectively are more likely to be satisfied with their care, to share crucial information to help get an accurate diagnosis, to adhere to recommendations, and to stick with recommended therapies9 in spite of negative side effects or not being able to see the effects of those therapies directly.
Using the science behind the “soft sciences” allows us to use data-based, actionable tools to achieve these shared patient and provider goals.
References
- Grau J, Wiegner R. One-stop cancer care; building a digitalized oncology center of excellence. In: Compendium – A world without fear of cancer. Insights Series Compendium. Siemens Healthineers. 2022;33:77-81.
- Vrinten C, McGregor LM, Heinrich M, et al. What do people fear about cancer? A systematic review and meta-synthesis. Lancet. 2014;384:S12.
- The Beryl Institute. Ipsos PX Pulse. Consumer perspectives on patient experiences in the U.S. November 2022. Accessed July 31, 2023. https://the berylinstitute.org/wp-content/uploads/woocommerce_uploads/2023/02/PXPulse_Q3_Nov2022-uvzyrx.pdf
- AHIMA Foundation Study. Understanding, access and use of health information in America. October 2021. Accessed July 14, 2023. https://ahima foundation.org/media/ngfbggsk/oct2021_understanding_access_use_health_information_america_ahima_foundation.pdf
- SAMHSA’s Concept of Trauma and Guidance for a Trauma-Informed Approach. July 2014. Accessed May 18, 2023. https://ncsacw.acf.hhs.gov/userfiles/files/SAMHSA_Trauma.pdf
- Evans O. Amygdala Hijack: How It Works, Signs, & How To Cope. Simply Psychology. Updated July 20, 2023. Accessed July 31, 2023. www.simplypsychology.org/amygdala-hijack.html
- Weber DL. Information processing bias in post-traumatic stress disorder. Open Neuroimag J. 2008;2:29-51.
- Medina J. Brain Rules: 12 Principles for Surviving and Thriving at Work, Home, and School. Pear Press. 2010.
- Moslehpour M, Shalehah A, Rahman FF, Lin KH. The effect of physician communication on inpatient satisfaction. Healthcare (Basel). 2022;10:463.
- Appold K. Communication tools improve patient experience and satisfactions. The Hospitalist. Published August 24, 2017. Accessed July 9, 2023. www.the-hospitalist.org/hospitalist/article/145285/transitions-care/com munication-tools-improve-patient-experience-and
- Moorey SS. Breast Cancer and Body Image. In: Nasser M, Baistoe, Treasure J, eds. The Female Body in Mind. Routledge. 2007.
- Lemieux J, Maunsell E, Provencher L. Chemotherapy-induced alopecia and effects on quality of life among women with breast cancer: a literature review. Psychooncology. 2008;17:317-328.
- Major B, Schmader T. Stigma, social identity threat, and health. In: Major B, Dovidio JF, Link BG, eds. The Oxford Handbook of Stigma, Discrimination, and Health. Oxford University Press; 2018:85-103.
- Maass SWMC, Roorda C, Berendsen A, et al. The prevalence of long- term symptoms of depression and anxiety after breast cancer treatment: a systematic review. Maturitas. 2015;82:100-108.
- Hunger J, Major B, Blodorn A, Miller C. Weighed down by stigma: how weight-based social identity threat contributes to weight gain and poor health. Soc Personal Psychol Compass. 2015;9:255-268.
- Carey K, Linaschke J. Beauty After Breast Cancer. No Scars No Stories; 2015.
- Perez-Tejada J, Aizpurua-Perez I, Labaka A, et al. Distress, proinflammatory cytokines and self-esteem as predictors of quality of life in breast cancer survivors. Physiol Behav. 2021;230:113297.
- Triantafyllou C, Alvarez IN, Gray M, Rowley N. Emotional care: the overloaded element in the cancer pathway. In: Compendium – A world without fear of cancer. Insights Series Compendium. Siemens Healthineers. 2022; 33:98-109.
- Slepian M, Jacoby-Senghor DS. Identity threats in everyday life: distinguishing belonging from inclusion. Social Psychological and Personality Science. 2021;12:392-406.
- Lloyd-Williams M. Depression—the hidden symptom in advanced cancer. J R Soc Med. 2003;96:577-581.
- The HIPAA Journal. Effects of poor communication in healthcare. Accessed August 12, 2023. www.hipaajournal.com/effects-of-poor-communica tion-in-healthcare/
- Mausbach BT, Yeung P, Bos T, Irwin SA. Health care cost of depression in patients diagnosed with cancer. Psychooncology. 2018;27:1735-1741.
Funding
Not applicable
Conflicts of Interest
The last 3 paragraphs under “Cognitive Science and Learning” make reference to a resource book that uses the principles mentioned throughout the article to redesign a standard patient resource. The author of this article is also the author of that book, which is sold at print cost (or often donated) through a not-for-profit breast cancer outreach effort. The book title is mentioned only in the reference list.
The author is founder of Beauty After Breast Cancer, Exeter, NH, USA.




