Patient navigators are widely used to guide patients through the healthcare maze, providing education, financial networking, expert clinical judgment, emotional support, timely access, and continuity of care. This review examines the outcomes of different types of navigators reported in 14 studies published between 2007 and 2013. These studies all showed positive outcomes associated with navigation in identifying and overcoming barriers and increasing the timeliness of care. However, the tools used to measure outcomes varied from study to study, many had not been tested for reliability and validity, and none focused on nurse-sensitive outcomes. In addition, it is difficult to directly compare patient outcomes between studies due to the lack of information about role definition and credentialing requirements of navigators. Finally, none of the studies focused on nurse-sensitive outcomes to test the effectiveness of nurse navigators.
The role of patient navigator was created in 1990 by Harold P. Freeman, MD, who recognized disparities in healthcare access for the underserved in New York City’s Harlem African American neighborhood.1 In Freeman’s 2012 article reviewing the origin, evolution, and principles of navigation, he notes that navigators in many settings have successfully alleviated many of the barriers to cancer care, resulting in an increase in access to treatment, timely diagnosis, and effective community outreach. All of these are considered navigator outcomes. Trained laypersons were frequently used rather than nurses, and Freeman notes that the role and training should vary depending on the setting and the population of patients served.1 Freeman also notes that the American College of Surgeons Commission on Cancer mandated that patient navigation is to be one of the standards of care for cancer programs beginning in 2015, and that Congress has mandated Medicaid payment for navigator services.
Today’s patient navigator guides patients through the healthcare maze, providing education, financial networking, expert clinical judgment, emotional support, timely access, and continuity of care. In 2010, Mary Ann B. Case, RN, MSN, OCN, published a review of 18 nursing studies measuring the effects of using an oncology nurse as a patient navigator.2 She reported several positive outcomes, including decreased time to diagnosis, decreased distress scores, improved aspects of quality of life, greater understanding of health problems, and greater patient satisfaction. While some of these are likely to be nurse-sensitive outcomes (ie, greater understanding of health problems), others may not need a nurse (ie, decreased distress score). In addition, Ms Case did not advocate for standardized tools measuring nurse- sensitive outcomes. And, unfortunately, studies conducted since Ms Case’s integrative review continue to lack consistency in role definition and minimal educational requirements of the patient navigator and in outcomes being measured. Consequently, it is difficult to determine whether the navigator’s credentials (eg, nurse or nonnurse) are a determinant in patient outcomes.
Despite evidence that links patient navigators to positive outcomes, there is ambiguity surrounding the role and definition of a patient navigator, including education and credentialing requirements, and a standard definition of the patient navigator role has yet to be determined. The Oncology Nursing Society (ONS) 2010 position paper on navigation notes that additional research must be done to explore, confirm, and advance navigation roles, and that metrics need to be developed to clarify the role, function, and desired outcomes of navigators. The ONS notes that earlier studies have recommended additional research on educational preparation, certification, and outcomes of navigators of all kinds.3 As a first step, this integrative review examines the most recent evidence of the outcomes of different types of navigators. A special focus was placed on the tools being used to measure navigator outcomes, as they vary from study to study.
Methods
The databases used to obtain research articles for the review included the Cumulative Index to Nursing and Allied Health Literature, PubMed, Google Scholar, and manual searches. In addition, research reports reference lists and related article links were reviewed. Key words searched used various combinations of patient navigation, roles, navigator, cancer, outcomes, continuity of care, timeliness, time to treatment, and nurse. In order to capture the most recent data, only articles published from 2007 to 2013 were included in the search. Articles were not limited to nursing research since the authors believed it was important to collect evidence from a broad range of resources.
Inclusion criteria for the review were peer-reviewed journal publications in English, available full text, research article, written in the United States, use of a type of navigator that was clearly defined, and reports of patient outcomes. In all of the studies, the patient navigator was considered the independent variable. The effects and outcomes of the navigator varied from study to study. Two studies were excluded because the primary focus was on instrument development and methodological issues in developing tools to measure patient satisfaction with navigation. These 2 studies will be discussed in the recommendations for practice. Fourteen studies met the inclusion criteria for this review.
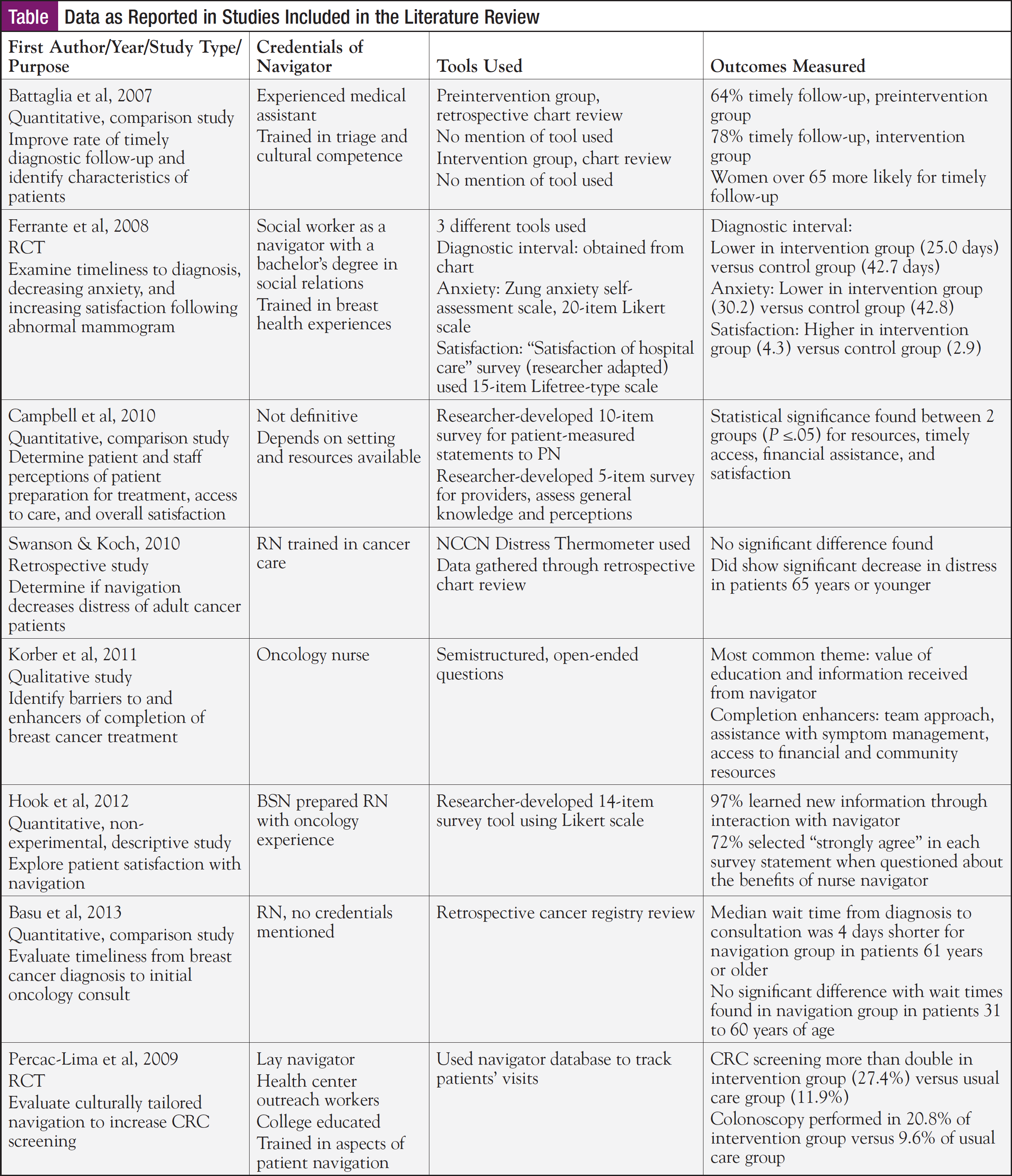
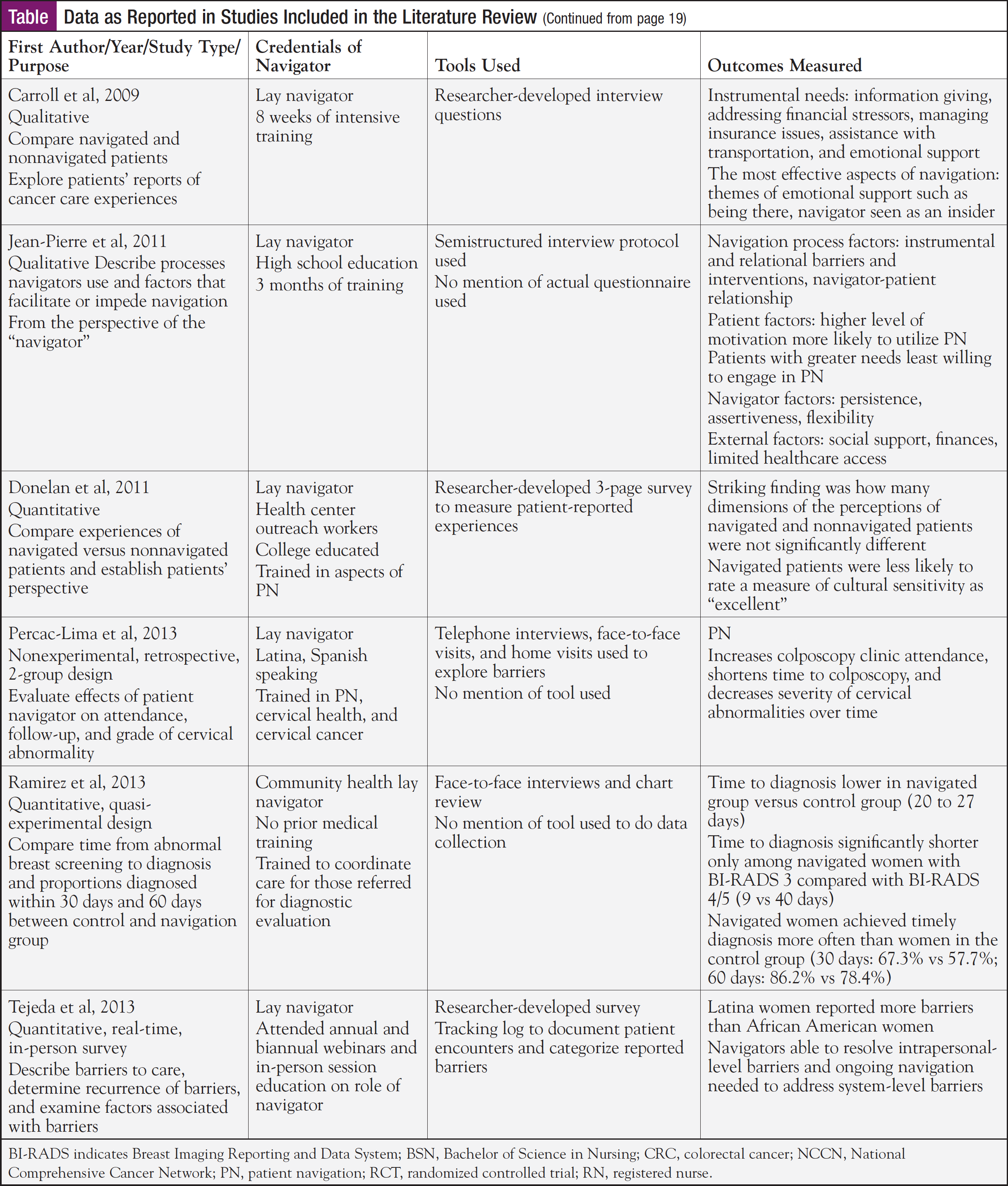
A matrix was created to analyze the studies. Authors, patient population and setting, type of study, purpose, credentials of the navigator, definition of the navigator, data collection method, tools used to collect data, outcomes/findings of the study, study limitations, and implications for nursing were included in the matrix. The matrix was very helpful in synthesizing participants and methods, navigator credentials and role, and outcomes of the 14 studies. The authors have included the following 3 columns from the original matrix (credentials, tools used, outcomes measured)—and have abbreviated the information in each of the columns in order to create a table that is suitable for publication. These findings from the matrix are summarized in the following paragraphs (Table).
Results
Participants and Setting
Overall, the number of participants in the studies included ranged from 13 to 1332. The studies were conducted at hospitals, community health centers, comprehensive community cancer centers, and outpatient clinics. The majority of the samples were drawn from urban settings in the northeastern part of the United States. Additional settings included the southeastern region and the Midwest; 2 studies did not specify their location. Half of the studies included all ethnic groups; however, 3 of the earliest studies limited the study participants to minorities4-6 and 2 of the most recent studies limited participants to the Latino population.7,8 The inclusion of minorities reflects the original patient navigator program, designed by Dr Freeman, to facilitate care of minority cancer patients1 and the 2010 position paper of the ONS.3
Eleven studies were quantitative while 3 were qualitative. Two of the quantitative studies were randomized controlled trials.4,6 Other quantitative studies included 3 comparison studies,5,9,10 a retrospective chart review,11 a nonexperimental descriptive study,10 a retrospective 2-study, quasi-experimental study,7 a real-time in-person survey,12 and an evaluative study.13
Three qualitative studies were included to capture subjective input and the human experience, both considered important aspects of patient navigation.14-16 One qualitative study examined navigated and nonnavigated patients’ reports of cancer care experiences.15 Another qualitative study focused on identification of barriers to and enhancers of completion of breast cancer treatment from the perspective of the patients.14 The third qualitative study sought to describe the key processes that navigators actually used from the perspective of the navigator.16 These different study designs resulted in the outcomes being measured varying from study to study, indicating that there is not a core set of evidence-based outcomes being measured.
Purpose of the Studies Reviewed
Patient navigation programs are driven by individual population needs.13 The purpose of the studies varied depending on the study population being addressed. The majority of the earlier studies limited the participants to minorities. These earlier studies measured timely diagnosis, levels of anxiety, satisfaction with care, and levels of screening.4-6 More recent studies explored the patients’ views of the impact of a patient navigator.9,10,14,15
The goal was to gain insight into the most effective and valuable aspects of patient navigation, patient preparation for treatment, overall impression of navigational services, and barriers/enhancers to completion of cancer treatment. Most recently, Sanja Percac-Lima, MD, PhD, and colleagues studied the impact of a culturally tailored navigator on cervical cancer prevention in the Latino population.8 Although significant positive outcomes were reported from the navigation group, Dr Percac-Lima placed little emphasis on the fact that the navigator was also Latina.8
Two studies examined the perspective of the healthcare providers. Pascal Jean-Pierre, PhD, MPH, and colleagues surveyed patient navigators in order to gain knowledge about the process they used when interacting with patients.16 The other study examined the staff members’ perceptions of how navigation impacted a patient’s preparation for cancer treatment.9
As the purpose varied from study to study, it is difficult to compare study findings. While it is useful to gain insight into the views of patients about navigation, using the same tools in every study may assist in meeting the call of the ONS to identify metrics to clarify the role, function, and desired outcomes of navigators.3
Methods Used in the Studies
Eight of the studies reviewed compared nonnavigated patients with navigated patients to determine if navigation had an impact on care.4-8,10,13,17 Two of these studies were randomized controlled trials.4,6 Three of the comparison studies reviewed patient charts retrospectively,5,7,17 and the qualitative studies conducted in-depth patient interviews.14-16
Navigator Credentials
Among the 14 studies reviewed, navigator credentials varied from study to study, making it difficult to determine which type of navigator results in which outcome. In 10 of the studies, the navigators were not nurses.4-10,12,15,16 Half of the studies used lay or community health workers for navigation, and in these 7 studies, training requirements varied considerably.6-8,10,12,15,16
Two studies using lay navigators had a high school diploma at a minimum. The navigators received extensive training in helping a patient through the healthcare system.7,16 In one study the lay navigators all had a college education.6 In addition, the navigators received 6 hours of training that included performing an initial interview to identify barriers and to address other aspects of patient navigation. The final 3 studies used navigators with varied backgrounds. Tracy A. Battaglia MD, MPH, and colleagues used a navigator who is a medical assistant.5 The medical assistant had minimal clinical experience but received training to help coordinate patient care.5
A navigator with a social work background was used by Jeanne M. Ferrante, MD, and colleagues.4 The navigator had a bachelor’s degree in social relations and received special training to assist patients with breast cancer. In the study by Cheryl Campbell, RN, BSN, ONC, and colleagues, the credentials of the navigator depended upon the setting and resources available; therefore, no specific credentials were listed.9 Patient navigator was used interchangeably with terms like nurse navigator, care coordinator, and case manager. The ONS recommends that either a nurse or social worker supervise nonprofessional navigators and volunteers.3 The navigators in 2 studies were supervised by a social worker.12,15 The navigators in another study were supervised by a social worker and a nurse practitioner,8 and in another by the study coordinator.5
Four studies employed nurses as navigators.11,13,14,17 Jay Swanson, RN, BSN, ONC, and colleagues were the only ones who provided an in-depth description of the nurse navigator’s training and background17; the others did not explicitly state the navigator’s qualifications. The investigators noted the nurses provided cancer education, supportive care, and appropriate referrals.
Definition of the Navigator Role
Although the credentials of the navigators varied from study to study, the definitions of the navigator role were similar in all 14 studies. In all, navigation encompassed a wide range of patient advocacy, identification of barriers to care, and coordination of care with the ultimate goal of high-quality care for individuals. Two studies identified navigation as a type of care management.5,14 In several other studies, the role of the navigator included provision of emotional and social support during the cancer journey.4,7,11,12,14,16,17 In addition, the importance of connecting patients with resources was addressed. Interestingly, only 4 of the studies identified patient education as part of the navigator role9,11,13,14 and 3 of these studies used nurses as navigators,11,13,14 which does provide some support that navigators be nurses.
Tools Used to Measure Effectiveness of Navigation
The tools used to gather data and types of data collected in the 14 studies varied considerably. Three studies gathered data through retrospective chart reviews,5,13,17 yet only 1 study noted that the project coordinator reviewed the data abstraction for completeness, accuracy, and internal consistency.5 Two of the studies collected data from navigator databases.6,13 Again, these databases may be assumed to be accurate, but the data were not confirmed with the patient records or patients themselves. In 3 of the quantitative studies, the investigators developed written survey tools9,11,12 and the 3 qualitative studies were interviews.14-16 While the investigators who developed the tools mentioned some tests of reliability and validity, each study used a different tool, and performed different reliability and validity tests.9,11,12
The investigators of 2 studies did use some standardized tools that have been tested for reliability and validity. One study measured anxiety using the Zung anxiety self-assessment scale.4 One study measured distress using the National Comprehensive Cancer Network (NCCN) Distress Thermometer.11 However, additional data were collected for both of these studies using researcher-developed tools that were not tested for reliability and validity.
Findings/Outcomes of Navigation
The findings/outcomes of navigation from the 14 studies can be grouped into 3 categories: identified barriers, navigation process and perceptions, and timeliness of care.
Identified barriers. Identification of barriers to care is an important aspect of patient navigation, because when barriers are identified, navigators can help the patient navigate the difficulties in the healthcare system more efficiently. Three studies, all using lay navigators, identified financial stressors, managing insurance issues, transportation issues, and lack of information/education as common barriers that affect patient care.12,15,16 A common theme in each of these studies was the need for emotional or social support from the navigator. In fact, Jennifer K. Carroll, MD, MPH, and colleagues found that emotional support was identified as the most effective aspect of navigation.15
Navigation process and perceptions. The process of navigation varied in different geographic settings, populations, and institutions. However, the principle of navigation was constant: navigation was developed to assist patients and families to help improve fragmented care, and ultimately to improve outcomes. Four studies examined the perception of navigation and the navigational process.10,11,14,17 With the use of a lay navigator, Daniel Donelan, PhD, and colleagues compared the experiences of navigated patients and nonnavigated patients. However, the perceptions did not significantly differ and many dimensions of the care received by the 2 groups were similar.10
A cancer diagnosis can cause a high level of distress in patients and their family members. Navigation is thought to alleviate some of this distress by offering contact with the navigator in many aspects of the patient’s care. Thus, using a nurse navigator, Jay Swanson and Lisa Koch sought to determine whether navigation decreased distress levels using the NCCN Distress scale in patients.17 No significant differences in level of distress were found in patients overall; however, there was a decrease in distress in patients 65 years of age or younger.
The value of education and information received from a nurse navigator was the most common theme found by Susan F. Korber, MS, RN, OCN, NE-BC, and colleagues. Patients in their study appreciated the team approach used in their care, which was facilitated by the nurse navigator. Also, assistance with managing cancer symptoms, cancer treatment, financial resources, and community resources were considered benefits of navigation.14 Similarly, in the study by Ann Hook, MSN, RN, and colleagues, 97% of navigated patients reported learning new information from their navigator; 71% to 90% “strongly agreed” with each statement on the benefits of the nurse navigator.11
Timeliness of care. The negative effects of delayed screening, follow-up of abnormal findings, and diagnosis were determining factors in the development of navigators to help improve patient outcomes. Historically, minorities and those with lower socioeconomic status were found to have later stages of cancer at time of diagnosis and worse survival rates. Navigation has been found to reduce this disparity.1 Seven of the studies reviewed here studied the effects of patient navigation on timeliness of screening, diagnostic follow-up, and diagnosis of cancer.4-9,13 Percac-Lima and colleagues conducted 2 studies examining whether patient navigation using lay navigators increased the number of patients who underwent cancer screening.6,8 Among navigated patients, the number who had colonoscopy screening was more than double that of nonnavigated patients: colonoscopy screening was performed in 20.8% of navigated patients and 9.6% of nonnavigated patients.6 Another positive effect of navigation was found in colposcopy clinic attendance and time to colposcopy. In the second study by Percac-Lima and colleagues using lay navigators, navigation increased the number of people who have timely colposcopies, thereby reducing the severity of cervical abnormalities.8
Timely follow-up after an abnormal finding is essential to improve cancer outcomes. All of these studies, regardless of the type of navigator, found that navigated patients had a shorter time to diagnosis than nonnavigated patients. In one study that used a medical assistant as navigator, 78% of navigated women had timely follow-up to diagnosis while only 64% of nonnavigated women had timely follow-up. Interestingly, women 65 years of age and older were more likely to have timely follow-up than women 18 to 39 years of age.5 In the study by Ferrante and colleagues, using a social worker as a navigator, women in the navigated group had a shorter interval to diagnosis than the nonnavigated group (25 days vs 42.7 days).4 A similar finding was reported in a study where the navigator credentials were not clearly defined.9 Navigated Latina patients with breast cancer were found to have an average of 20 days from time of abnormal finding to diagnosis versus 27 days for nonnavigated patients.7 In this study, the lay navigator had no prior medical training.
One study, using a nurse as a navigator, focused on the time from diagnosis to consultation.13 For patients 61 years of age and older, the median wait time from diagnosis to consultation was 4 days shorter with navigation than without navigation (8 days vs 12 days). However, for patients 31 to 60 years of age, navigation was not a significant predictor of reduced wait times (9 days vs 10 days).13
Discussion
This review examined different types of navigators and patient outcomes of navigation. Overall, the use of a patient navigator was linked to positive outcomes, including identification of barriers, positive perceptions of the navigation processes, timeliness of care, timely follow-up, and decreased levels of distress.
The type of navigator used was not found to affect patient outcomes. However, direct comparison of studies was difficult, because the tools used to measure the outcomes were not designed to capture specific outcomes unique to the role of patient navigators.
Navigators have been used since the 1990s, but in order to advance the science of navigator effectiveness, standardized tools for data collection are needed that have been tested for reliability and validity. In addition, if the same variables such as distress, anxiety, and patient satisfaction were measured in every study, using the same instruments, then the effects of different types of navigators could be detected.
The findings from this review reinforce the need to define the role and educational requirements for a patient navigator, and then to use reliable and valid tools to measure the unique effects of navigators with different roles, different training, and in different settings. Two methodological studies found good reliability and validity scores of the “patient satisfaction with interpersonal relationship with navigator measure” (PSN-1).18,19 One was a multisite study,18 and the second tested a Spanish version of the tool.19 The use of this tool in all future studies of navigators would provide standardized data on patient satisfaction that is specific to the navigator role. The correlation of patient satisfaction, type of navigator, and outcomes, such as timeliness of care, would be possible using the PSN-1.
Limitations
There are some limitations to this review. A number of the studies focused on particular populations, typically underserved, low-income minorities, which limits generalizability to the broader population. Another limitation involved the use of researcher-developed instruments with little or no discussion of the reliability and validity of the data collected. Also, collection of data retrospectively potentially contributes to poorer quality data. Despite these limitations, the studies reviewed have implications for nursing practice and nursing research.
Implications for Nursing Practice and Nursing Research
Four of the studies reviewed employed nurses as navigators, and their implications are reported here. Swanson and Koch pointed to the need for oncology nurse navigators to prioritize workloads given the stronger impact these navigators had on patients less than 65 years of age.17
In addition, they concluded that some patients may require navigational contact with each healthcare encounter. Korber and colleagues noted that the primary objectives of nurse navigation were to increase the number of cancer care treatment completions in women with breast cancer, and reduce the prevalence of fragmented care.14 Hook and colleagues suggested that using nurses in the navigation role has the potential to offer promising resolution of patient care inadequacies. They stressed the importance of identifying key components of effective navigation programs in solving this problem.17 Mouha Basu, MPH, and colleagues noted that further examination of the patient navigation processes could help identify methods to improve timely care for patients.13
The tools currently used to evaluate the effectiveness of patient navigators are not designed to capture the essence of what a nurse navigator does compared with navigators who are “laypeople” or social workers. In order to capture this data, nurse-sensitive outcomes need to be clearly defined, and then specifically evaluated. For example, it is important to determine whether nurses are more effective than others in assisting patients to make treatment decisions, more effective in convincing patients to seek follow-up, and more effective in helping patients to cope with and overcome the effects of chemotherapy. In acute care, the rates of nosocomial infections and pressure ulcers are considered nurse-sensitive outcomes. What are the nurse-sensitive outcomes for cancer outpatients? The ONS position paper does not specifically identify what the appropriate, nurse-sensitive, evidence-based outcome measures should be.3
Many other questions need to be addressed in order to evaluate whether a nurse needs to be a navigator. It may be that a group of 3 to 5 layperson navigators could meet regularly with 1 nurse navigator to review the caseload and is available for referral when the special knowledge and experience of a nurse is needed. In addition, there may be a role for an advanced practice navigator who not only helps patients with education, financial networking, emotional support, and timely access and continuity of care, but also uses expert clinical judgment to diagnose and treat some of the clinical manifestations patients experience as they go through cancer treatment. This advanced practice nurse could be especially helpful with end-of-life care planning, and help to overcome the problem of too short a stay in palliative care and hospice care.
Conclusion
The evidence supporting the use of patient navigators, not only for cancer patients but also patients with other chronic diseases, continues to grow. Despite the positive outcomes of identifying and overcoming barriers, emotional support, and timeliness of care associated with patient navigation, there is still a paucity of information on role definition and credentialing requirements.
Future research can be directed toward designing studies that compare the outcomes of nurse navigators, lay navigators with minimal training, and lay navigators with comprehensive training, using tools that have been tested for reliability and validity. This review suggests that the ONS 2010 call to identify metrics to clarify the role, function, and outcomes of navigators has not been answered.3
Additional nursing research with tools designed to capture nurse-sensitive outcomes is also needed to address the unique role nurse navigators can play as patient advocates, educators, and facilitators.
Acknowledgment
The authors gratefully acknowledge the inspiration, vision and editorial assistance of Elizabeth Tornquist, MA, FAAN, with this manuscript.
Author Disclosure Statement: All authors have nothing to disclose.
Corresponding Author: Donald D. Kautz, RN, PhD, CRRN, CNE, ACNS-BC, Associate Professor of Nursing, The University of North Carolina at Greensboro, PO Box 26170, Greensboro, NC 27402-6170. E-mail: This email address is being protected from spambots. You need JavaScript enabled to view it..
References
- Freeman HP. The origin, evolution, and principles of patient navigation. Cancer Epidemiol Biomarkers Prev. 2012;21(10):1614-1617.
- Case MA. Oncology nurse navigator: ensuring safe passage. Clin J Oncol Nurs. 2011;15(1):33-40.
- Oncology Nursing Society. Oncology Nursing Society, the Association of Oncology Social Work, and the National Association of Social Workers joint position on the role of oncology nursing and oncology social work in patient navigation. www.ons.org/about-ons/ons-position-statements/education-certification-and-role-delineation/oncology-nursing-0. Accessed February 26, 2014.
- Ferrante JM, Chen PH, Kim S. The effect of patient navigation on time to diagnosis, anxiety, and satisfaction in urban minority women with abnormal mammograms: a randomized controlled trial. J Urban Health. 2008;85(1): 114-124.
- Battaglia TA, Roloff K, Posner MA, Freund KM. Improving follow-up to abnormal breast cancer screening in an urban population: a patient navigation intervention. Cancer. 2007;109(2 suppl):359-367.
- Percac-Lima S, Grant RW, Green AR, et al. A culturally tailored navigator program for colorectal cancer screening in a community health center: a randomized, controlled trial. J Gen Intern Med. 2009;24(2):211-217.
- Ramirez AG, Perez-Stable EJ, Penedo FJ, et al. Navigating Latinas with breast screen abnormalities to diagnosis: the Six Cities Study. Cancer. 2013;119 (7):1298-1305.
- Percac-Lima S, Benner CS, Lui R, et al. The impact of a culturally tailored patient navigator program on cervical cancer prevention in Latina women. J Womens Health (Larchmt). 2013;22(5):426-431.
- Campbell C, Craig J, Eggert J, Bailey-Dorton C. Implementing and measuring the impact of patient navigation at a comprehensive community cancer center. Oncol Nurs Forum. 2010;37(1):61-68.
- Donelan K, Malihot JR, Dutwin D, et al. Patient perspectives of clinical care and patient navigation in follow-up of abnormal mammography. J Gen Intern Med. 2011;26(2):116-122.
- Hook A, Ware L, Siler B, Packard A. Breast cancer navigation and patient satisfaction: exploring a community-based patient navigation model in a rural setting. Oncol Nurs Forum. 2012;39(4):379-385.
- Tejeda S, Darnell JS, Cho YI, Strolley MR, Markossian TW, Calhoun EA. Patient barriers to follow-up care for breast and cervical cancer abnormalities. J Womens Health. 2013;22(6):507-517.
- Basu M, Linebarger J, Gabram SG, Patterson SG, Amin M. Ward KC. The effect of nurse navigation on timeliness of breast cancer care at an academic comprehensive cancer center. Cancer. 2013;19(14):2524-2531.
- Korber SF, Padula C, Gray J, Powell M. A breast navigator program: barriers, enhancers, and nursing interventions. Oncol Nurs Forum. 2011;38(1):44-50.
- Carroll JK, Humiston SG, Meldrum SC, et al. Patients’ experiences with navigation for cancer care. Patient Educ Couns. 2010;80(2):241-247.
- Jean-Pierre P, Hendren S, Fiscella K, et al. Understanding the process of patient navigation to reduce disparities in cancer care: perspectives of trained navigators from the field. J Cancer Educ. 2011;26(1):111-120.
- Swanson J, Koch L. The role of the oncology nurse navigator in distress management of adult inpatients with cancer: a retrospective study. Oncol Nurs Forum. 2010;37(1):69-76.
- Jean-Pierre P, Fiscella K, Winters PC, et al. Psychometric development and reliability analysis of a patient satisfaction with interpersonal relationship with navigator measure: a multi-site patient navigation research program study. Psychooncology. 2012;21(9):986-992.
- Jean-Pierre P, Fiscella K, Winters PC, et al. Cross-cultural validation of a patient satisfaction with interpersonal relationship with navigator measure: a multi-site patient navigation research study. Psychooncology. 2012;21(12):1309-1315.