Background: Medication adherence is a key contributor to survival for patients with chronic myeloid leukemia (CML). About 25% to 35% of CML patients have been reported to have suboptimal medication adherence.
Objectives: Guided by psychobehavioral theory, the purpose of this research was to characterize oral CML medication adherence by specifically considering patients’ financial burden and psychosocial distress. We hypothesized that psychosocial distress modulates the impact of financial burden on oral adherence to CML medication (self-reported).
Methods: Data for this study are from the Cancer Support Community's Cancer Experience Registry: CML, which is an online research initiative. Patients were asked about financial burden, psychosocial distress, and medication adherence. The total analytic sample included 318 patients with CML.
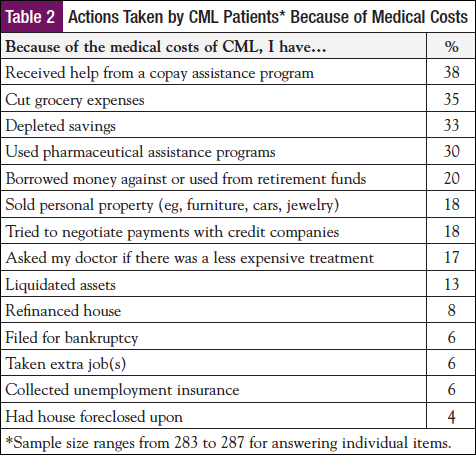
Results: Thirty-one percent of patients were categorized as having suboptimal CML medication adherence. Using a regression model, there was a significant interaction between financial burden and high risk of depression on treatment adherence (P = .024; n = 262). Adjusting for age and income, patients experiencing financial burden and at high risk for depression were significantly more likely to have suboptimal adherence than patients experiencing only financial burden.
Discussion: To help ensure optimal benefit from CML therapy, it is essential to develop and evaluate interventions that foster patient-clinician communication and referral for services related to both financial need and psychosocial distress.
Conclusion: Addressing adherence to CML medications through assessment of individual financial and psychosocial aspects of care is vital to help ensure optimal adherence and best possible treatment outcomes.
An estimated 8220 new cases of chronic myeloid leukemia (CML) were expected for 2016, representing more than 10% of all expected new leukemia cases.1,2 Advances in CML therapy with oral medications have transformed CML from an often fatal form of cancer to a highly manageable chronic condition.3,4 Based on estimates of survival with currently available therapies, the prevalence of CML is projected to be upward of 200,000 people by 2050.5
Addressing adherence to CML medications is vital; suboptimal adherence is associated with adverse outcomes, namely, treatment failure and increased healthcare costs.6-9 Currently, the National Comprehensive Cancer Network recommends that CML patients who are responding to and tolerating oral CML medications should remain on treatment indefinitely.10 Yet, 25% to 35% of CML patients have been reported to have suboptimal medication adherence, which has been defined in the literature in a number of ways, including the use of ≤85% or 90% of prescribed drug.11
A fuller understanding of the factors contributing to suboptimal medication adherence among CML patients will allow for the development of effective interventions. To date, a small but developing body of literature names several factors that contribute to CML patient medication adherence: increased clinician and patient knowledge about CML and its treatment, monitoring of adverse events by clinicians, and taking other medications for chronic conditions are associated with better adherence.8,12 In contrast, factors such as younger age, living alone, male gender, having medication side effects, a longer time between diagnosis and treatment, a longer time on treatment, and poor side effects management are associated with suboptimal adherence.8,9,12 Another factor that may foster suboptimal adherence is the direct cost of CML treatment. At least 1 study shows that patients with higher copayments for oral CML medication are more likely to discontinue their medication or be nonadherent to treatment in other ways.13
The effects of untreated distress in cancer patients, including suboptimal treatment adherence, medical outcomes, and quality of life (QOL), have been documented.14 However, the impact of distress levels among CML patients has not been systematically explored despite evidence that CML patients experience deficits in QOL and heightened distress.15,16 For example, patients taking oral CML medications for an average of 4 years reported more depression, anxiety, fatigue, and symptom burden and worse physical QOL compared with age- and gender-matched controls with no history of cancer.16
We investigated the relationship between oral medication adherence and financial burden combined with psychosocial distress; we were guided by psychobehavioral theory that postulates the extent to which individuals are able to modulate and regulate their emotion around stressors and how that impacts behavior.17-19 Specifically, we explored the extent to which psychosocial distress modulates the impact of financial burden on adherence to oral CML medication (self-reported).
Methods
Data for this study come from the Cancer Support Community’s (CSC) Cancer Experience Registry, which is a research initiative designed to collect the social and emotional experiences of cancer patients. The registry currently comprises 10 subregistries, including one for CML. For the Cancer Experience Registry: CML, CML-specific questions were developed by staff at the CSC and the Leukemia & Lymphoma Society (LLS) in conjunction with an advisory council consisting of clinicians, researchers, people living with CML, and other advocacy organizations. Registrants were recruited through outreach to CSC and LLS networks of community-based affiliates and chapters, online communities, CSC Helpline and LLS Information Resource Center, other advocacy organizations, and social and other media channels. An independent institutional review board (IRB), Ethical and Independent Review Services, conducted an ethics review and provided an IRB waiver. Registrants provided consent through an online process. From October 2013 to June 2014, 484 patients with CML registered for the Cancer Experience Registry: CML. A total of 393 registrants provided informed consent and participated in a web-based survey. We excluded survey participants living outside the United States (n = 55) and participants who were not currently taking oral CML medication (n = 20), resulting in a total analytic sample size of 318.
We collected the following information relevant to this analysis through the Cancer Experience Registry: CML.
Background Variables
Patient Characteristics
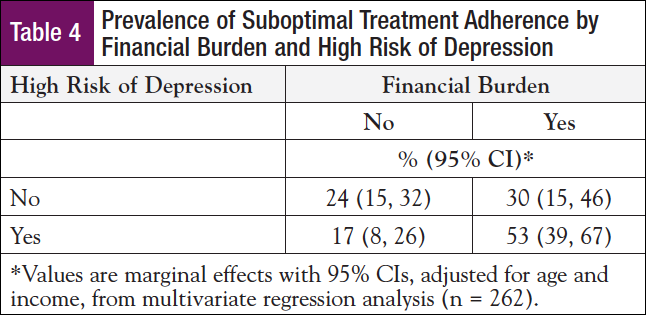
The following self-reported sociodemographic variables were collected: age, gender, race/ethnicity, education, household income, and time since CML diagnosis (Table 1).
 Independent Variables
Independent Variables
Financial Cost of CML
For 32 items, patients were asked to respond by indicating “yes” or “no” to the following statement: “Because of the medical costs of CML, I have….” Examples of these items include: taken an extra job(s); foregone vacations, celebrations, and social events; downsized my living accommodations; cut my grocery expenses; depleted savings; borrowed against or used money from retirement funds; and used copay assistance program. We developed a measure for “financial burden” drawn from 2 items: (1) depleted savings, and (2) borrowed against or used money from retirement funds; these were chosen given their relevance to immediate and future financial status. Financial burden was evident if a respondent indicated “yes” for either item. In addition, we analyzed the use of copay assistance programs and cutting grocery expenses in relation to adherence as proxy measures for short-term financial burden.
Psychosocial Distress
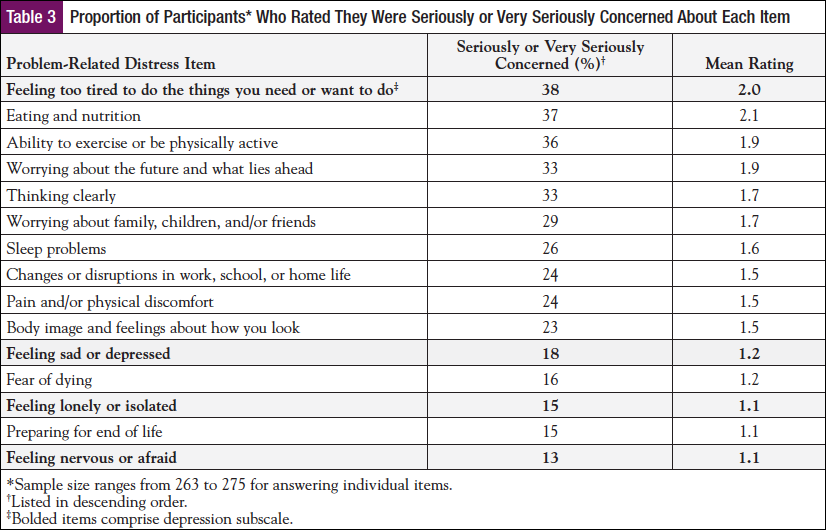
We incorporated 2 different measurements of psychosocial distress. First, to measure stress-related “intrusive ideation” about managing the financial impact of living with CML, patients completed the Impact of Event Scale20 intrusion subscale (7 items, each scored 0 for “not at all,” 1 for “rarely,” 3 for “sometimes,” and 5 for “often”). Items included, “I thought about it when I didn’t mean to”; “other things kept making me think about it”; and, “any reminder brought back feelings about it.” An intrusion score is calculated as the sum of the 7 items, and levels >13 were used to indicate clinically significant symptoms associated with anxiety.20 Second, patients completed a 4-item depression subscale (feeling sad or depressed, feeling lonely or isolated, feeling nervous or afraid, feeling too tired to do the things you need or want to do) from the CancerSupportSource distress screening tool.21 For each item, respondents are asked to indicate, “Today, how concerned are you about…?” (0 = not at all, 1 = slightly, 2 = moderately, 3 = seriously, 4 = very seriously). The items (α = 0.88) were summed for a depression score with a dichotomous variable indicating “high risk of depression” (yes or no based on a score ≥6).
Outcome Variables
Medication Adherence
Respondents were asked to classify the frequency of missing a dose of their oral CML medication as never, once per month, 2 times per month, once per week, or several times per week. Using a 5-point Likert scale (never, rarely, sometimes, often, always), respondents were also asked to indicate how often they postponed filling prescriptions, and how often they skipped doses of prescribed CML medications to reduce their healthcare spending. We defined “suboptimal medication adherence” as whether a patient endorsed any problems with adherence, which is consistent with the literature,8,22 and operationalized suboptimal adherence as having performed one or more of the following: (1) missed dose of oral CML medication more than once per month; (2) postponed filling prescriptions (responding either sometimes, often, or always); or (3) skipped doses of prescribed medications to reduce healthcare spending (sometimes, often, or always). “Suboptimal medication adherence” is dichotomous (yes or no).
Statistical Analysis
We performed descriptive analyses to characterize the patient sample, financial cost of CML, psychosocial distress, and CML medication adherence. We used Spearman’s rank correlation and chi-square tests to examine bivariate relationships between ordinal and dichotomous variables, respectively. We used logistic regression to examine the relationship between financial burden and medication adherence and to test for a mediation effect or effect modification of distress. We used a combination of bivariate and residual analyses to identify which measures for distress (intrusive ideation or depression) and financial cost of CML (financial burden, copay assistance, or cutting grocery expenses) were appropriate for model specification related to adherence. We used likelihood ratio tests and pseudo R-squared to indicate which model better predicts adherence. Age and income were included to adjust for potential confounding because they were significantly associated with adherence and at least 1 exploratory variable of interest. For age and income, we included a category for missing responses. All analyses used Stata 11.2. Using the predictive margins option in Stata, we reported the marginal effects from adjusted models. Probability estimates of P <.05 were considered statistically significant.
Results
Sample Characteristics
These patients with CML (n = 318) were predominantly female (68%), Caucasian (90%), 56 years of age on average (range, 18-85 years), and 5.2 years from their CML diagnosis. Additional characteristics are provided in Table 1.
Financial Cost Among the CML Patients
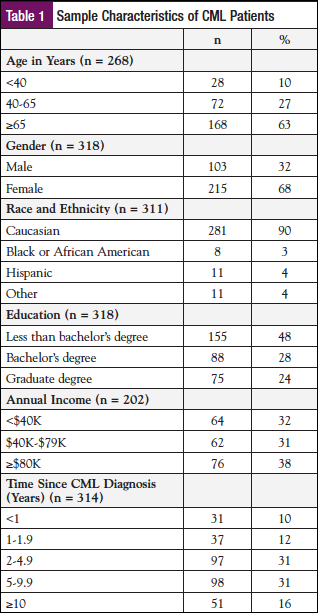
Nearly half (49%) of the CML patients reported spending at least $100 per month in out-of-pocket costs related to CML; 27% spent $250 or more; 16% spent $500 or more; 6% spent $1000 or more (Figure). One-third (34%) of patients reported that CML-related out-of-pocket costs affected their household “quite a bit” or “very much”; 22% responded “a little bit”; 26% responded “not at all.” Half (51%) of participants did not know if they were eligible for Social Security Disability Insurance or Supplemental Security Income, and 44% wished they had received more help with getting financial advice and assistance. To reduce the cost of CML, 23% (sometimes, often, or always) postponed seeking psychological counseling or support to reduce healthcare costs, 17% delayed follow-up on recommendations on complementary treatment, and 16% postponed doctor’s appointments.
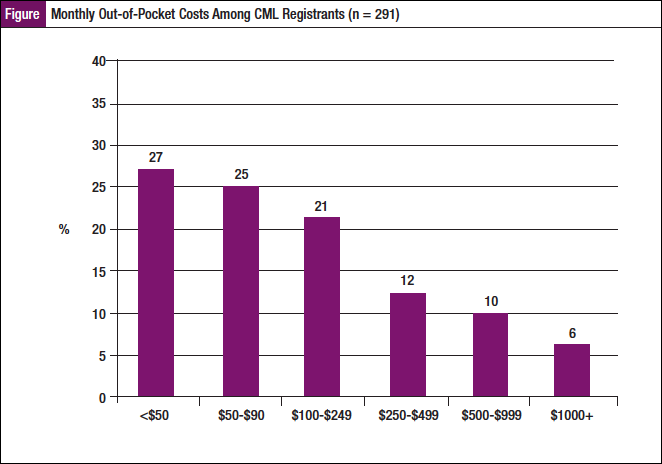
Because of the medical costs of CML, 33% reported depleting their savings, 20% borrowed against or used money from retirement, 38% indicated they had used copay assistance programs, and 35% reported cutting their grocery expenses (Table 2). More than one-third (35%) reported financial burden as defined by having either depleted savings or borrowed money from retirement funds.
Psychosocial Distress Among the CML Patients
The top concerns among the CML patients were feeling too tired to do the things you need or want to do (38%), eating and nutrition (37%), exercising and being physically active (36%), worrying about the future and what lies ahead (33%), and thinking clearly (33%) (Table 3). The mean score for intrusive ideation about the financial cost of cancer was 10.4 (SD = 9.8; n = 273), with 37% categorized as having clinically significant levels of anxiety (>13). Elevated depression was also evident in that the mean depression score for the patients was 5.5 (SD = 4.3; n = 266), and 45% were classified as being at high risk for depression (score >6).
Treatment Adherence
Among the CML patients, 10% reported skipping doses of oral CML drugs at least sometimes, 14% postponed filling prescriptions to reduce healthcare costs, and 19% reported missing a dose of oral CML drugs at least monthly. Thirty-one percent of the patients were categorized as having suboptimal medication adherence to their CML medication.
Financial Burden and Psychosocial Distress Impact Treatment Adherence
In the regression model testing main effects, financial burden was significantly associated with suboptimal treatment adherence (P <.001), but high risk of depression was not (P = .58). There was a significant interaction between financial burden and high risk of depression on suboptimal treatment adherence (P = .024; n = 262), adjusting for age and income. Among patients who experienced both financial burden and a high risk of depression, 53% (57% unadjusted) demonstrated suboptimal treatment adherence, meaning they skipped or missed doses of their oral CML drug or postponed filling prescriptions (Table 4). Among patients who experienced financial burden but were not at risk for depression, 30% (32% unadjusted) had suboptimal adherence. Similarly, 17% (18% unadjusted) of patients who were at risk for depression but did not experience financial burden had suboptimal medication adherence. Among those who did not experience financial burden or a high risk of depression, 24% (21% unadjusted) demonstrated suboptimal adherence. Stated another way, financial burden was significantly associated with poor adherence among those at risk for depression (odds ratio [OR] = 7.6; P <.001) but not among those not at risk for depression (OR = 1.3; P = .60).
Discussion
This study reinforces findings that patients with CML are experiencing financial and emotional strain. Prior literature shows that the financial challenges of cancer can have a strong negative impact, including lower adherence to treatment.9 We found that nearly half (49%) of the patients in this analysis reported spending $100 or more per month for out-of-pocket costs related to CML, while in turn 16% to 23% indicated postponing certain elements of care because of costs. Thus, patient-reported costs might translate into delay of potentially helpful or necessary care. More than one-third (35%) reported financial burden as defined by having either depleted savings or borrowed money from retirement funds, which demonstrates concern even for those who had grown their income over time. Depleting savings and retirement funds can have negative, long-term consequences in which patients experience lasting strain associated with financial burden.
The literature notes that CML patients are experiencing deficits in psychosocial health (ie, QOL, depressive symptoms).15,16 Our analysis confirms elevated distress among CML patients based on 2 measures for psychosocial distress that are strongly correlated but theoretically represent different domains of psychosocial distress. In our sample, 45% were classified as being at high risk for depression. Furthermore, patients in the sample had a mean score of 10.4 (SD = 9.8) for intrusive ideation about the financial cost of cancer, and 37% were categorized as having clinically significant levels of anxiety.
As suggested by psychobehavioral theory and noted in previous research, psychosocial factors can impact adherence.18,19,23-27 Indeed, 31% of the patients were categorized as having suboptimal CML medication adherence. And, importantly, the significant interaction between financial burden and high risk of depression on suboptimal medication adherence was evident, even when adjusting for age and income. Specifically, those patients experiencing financial burden and at high risk for depression are approximately 1.5 times more likely to have suboptimal adherence than patients who are experiencing only financial burden. Demonstrating that this effect on treatment is heightened among patients at risk for depression is an important addition to the CML literature.
Our results suggest that to enhance patients’ full benefit from CML therapy, it is essential to address the psychosocial well-being of patients. We found that patients with both financial burden and risk for depression were more likely to have suboptimal medication adherence (self-reported). Proactively screening patients for psychosocial distress and delivering appropriate follow-up intervention as a routine part of comprehensive care can be an effective strategy, along with developing and evaluating interventions that facilitate patient-clinician communication about treatment adherence, as well as screening and referral for financial concerns.23
The findings are especially meaningful considering the vast improvement in survivorship offered by CML oral medications; a steadily increasing number of patients will bear a significant financial strain given the need to stay on treatment indefinitely, as well as to meet the burden of ever greater cost sharing with higher copays and coinsurance, if current healthcare reimbursement trends continue.
We note several limitations and considerations with this research. Similar to other research, we did not use a validated tool to capture adherence. Instead, we used 3 survey questions to create a proxy measure for treatment adherence. Yet, the rate of suboptimal adherence identified in this study falls within the stated range identified in the literature. Our measure of financial burden was defined using information about depleted savings and borrowing against retirement accounts. This approach differs from prior approaches focused on out-of-pocket healthcare spending24-26 and may miss expenditures that were not supported by bank or retirement account savings. However, the consideration of withdrawals from savings may be more relevant for cancer patients.27,28 This study does not explore longitudinal effects associated with the impact on future income streams. The long-term financial implications of these short-term decisions warrant further study. In addition, the definition of financial burden and its relationship to adherence may differ across demographic populations.29 It should be noted that this patient sample had a higher ratio of female patients (68%) than what is consistent with CML population statistics and does not reflect ethnically or racially diverse populations; as such, these cross-sectional data cannot be generalized to other CML populations. Future studies are needed to understand and address underrepresented populations.
Conclusion
This research represents an important step toward understanding the impact of financial burden and psychosocial distress on medication adherence for CML patients. It suggests that future research in this area is appropriate and needed. Future research should incorporate longitudinal analyses on cost, distress, and drug adherence as well as explore potential interventions among a broader, more representative sample of CML patients. This research also provides important clinical relevance in that it underscores the importance of the oncology nurse navigator’s role in discussions with patients, and in assessment, support, and referral with regard to financial and psychosocial stressors relating to adherence to therapy.
References
- Howlader N, Noone AM, Krapcho M, et al, eds. SEER Cancer Statistics Review, 1975-2011. Bethesda, MD: National Cancer Institute. http://seer.cancer.gov/csr/1975_2011/. 2014. Accessed February 1, 2015.
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66:7-30.
- Jabbour E, Kantarjian H. Chronic myeloid leukemia: 2014 update on diagnosis, monitoring, and management. Am J Hematol. 2014;89:547-556.
- Siegel R, DeSantis C, Virgo K, et al. Cancer treatment and survivorship statistics, 2012. CA Cancer J Clin. 2012;62:220-241.
- Huang X, Cortes J, Kantarjian H. Estimations of the increasing prevalence and plateau prevalence of chronic myeloid leukemia in the era of tyrosine kinase inhibitor therapy. Cancer. 2012;118:3123-3127.
- Marin D, Bazeos A, Mahon FX, et al. Adherence is the critical factor for achieving molecular responses in patients with chronic myeloid leukemia who achieve complete cytogenic responses on imatinib. J Clin Oncol. 2010;28:2381-2388.
- Di Bella NJ, Bhowmik D, Bhor M, et al. Association between treatment adherence and response among patients with chronic myeloid leukemia (CML) receiving first-line TKIs in the community setting. Blood. 2013;122:2733.
- Noens L, Hensen M, Kucmin-Bemelmans I, et al. Measurement of adherence to BCR-ABL inhibitor therapy in chronic myeloid leukemia: current situation and future challenges. Hematologica. 2014;99:437-447.
- Jabbour E, Saglio G, Radich J, et al. Adherence to BCR-ABL inhibitors: issues for CML therapy. Clin Lymphoma Myeloma Leuk. 2012;12:223-229.
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines). Chronic Myelogenous Leukemia. 2014. www.nccn.org/professionals/physician_gls/f_guidelines.asp. Published 2014. Accessed February 1, 2015.
- Oehler VG. Update on current monitoring recommendations in chronic myeloid leukemia: practical points for clinical practice. Hematology Am Soc Hematol Educ Program. 2013;2013:176-183.
- Abraham I, MacDonald K. Why are patients with chronic myeloid leukaemia (non-)adherent? Br J Cancer. 2012;107:901-903.
- Dusetzina SB, Winn AN, Abel GA, et al. Cost sharing and adherence to tyrosine kinase inhibitors for patients with chronic myeloid leukemia. J Clin Oncol. 2014;32:306-311.
- Estes JM, Karten C. Nursing expertise and the evaluation of psychosocial distress in patients with cancer and survivors. Clin J Oncol Nurs. 2014;18:598-600.
- Trask PC, Cella D, Powell C, et al. Health-related quality of life in chronic myeloid leukemia. Leuk Res. 2013;37:9-13.
- Phillips KM, Pinilla-Ibarz J, Sotomayer E, et al. Quality of life outcomes in patients with chronic myeloid leukemia treated with tyrosine kinase inhibitors: a controlled comparison. Support Care Cancer. 2013;21:1097-1103.
- Miller SM, Shoda Y, Hurley K. Applying cognitive-social theory to health-protective behavior: breast self-examination in cancer screening. Psychol Bull. 1996;119:70-94.
- Miller SM, Buzaglo JS, Simms SL, et al. Monitoring styles in women at risk for cervical cancer: implications for the framing of health-relevant messages. Ann Behav Med. 1999;21:27-34.
- Leventhal H, Diefenbach M. The Active Side of Illness Cognition. In: Skelton JA, Croyle RT, eds. Mental Representation in Health and Illness. New York, NY: Springer-Verlag; 1991:247-272.
- Horowitz M, Wilner N, Alvarez W. Impact of event scale: a measure of subjective stress. Psychosom Med. 1979;41:209-218.
- Miller MF, Mullins CD, Onukwugha E, et al. Discriminatory power of 25-item distress screening tool: a cross-sectional survey of 251 cancer survivors. Qual Life Res. 2014;23:2855-2863.
- Greer JA, Amoyal N, Nisotel L, et al. A systematic review of adherence to oral antineoplastic therapies. Oncologist. 2016;21:354-376.
- Gater A, Heron L, Abetz-Webb L, et al. Adherence to oral tyrosine kinase inhibitor therapies in chronic myeloid leukemia. Leuk Res. 2012;36:817-825.
- Parish SL, Thomas KC, Williams CS, et al. Autism and families’ financial burden: the association with health insurance coverage. Am J Intellect Dev Disabil. 2015;120:166-175.
- Galbraith A, Wong ST, Kim SE, et al. Out-of-pocket financial burden for low-income families with children: socioeconomic disparities and effects of insurance. Health Serv Res. 2005;40(6 Pt 1):1722-1736.
- Galbraith A, Sinaiko AD, Soumerai SB, et al. Some families who purchased health coverage through the Massachusetts Connector wound up with high financial burdens. Health Aff (Millwood). 2013;32:974-983.
- Timmons A, Gooberman-Hill R, Sharp L. The multidimensional nature of the financial and economic burden of a cancer diagnosis on patients and their families: qualitative findings from a country with a mixed public-private healthcare system. Support Care Cancer. 2013;21:107-117.
- Timmons A, Gooberman-Hill R, Sharp L. “It’s at a time in your life when you are most vulnerable”: a qualitative exploration of the financial impact of a cancer diagnosis and implications for financial protection in health. PLoS One. 2013;8:e77549.
- Céilleachair AÓ, Costello L, Finn C, et al. Inter-relationships between the economic and emotional consequences of colorectal cancer for patients and their families: a qualitative study. BMC Gastroenterol. 2012;12:62.