Memphis, TN—One of the most popular breakout sessions at the Fourth Annual Conference of the Academy of Oncology Nurse & Patient Navigators (AONN+) focused on breast cancer navigation and survivorship. This session featured 2 speakers, Karen Meneses, PhD, RN, FAAN, and Vinnie Myers, a tattoo artist.
Breast Cancer Survivorship Initiatives
After recalling a hilarious personal anecdote related to her experience with stick-on nipples for her breast prostheses, Lillie Shockney introduced Dr Meneses, Professor and Associate Dean for Research at the University of Alabama at Birmingham (UAB) School of Nursing.
Dr Meneses is an internationally recognized nurse scientist in cancer survivorship. In 2013, she was appointed to the Centers for Disease Control and Prevention (CDC) Advisory Committee on Breast Cancer in Young Women. Most recently, Dr Meneses created the Young Breast Cancer Survivorship Network (YBCSN), which aims to improve the quality of life (QOL) for young breast cancer survivors and their loved ones through education, personal support, distance learning, and networking.
During the AONN+ meeting, Dr Meneses, an oncology nurse who has been in practice for nearly 40 years, shared her unique experience developing and evaluating educational interventions for breast cancer survivors in the Southeast.
To underscore the need for breast cancer survivorship initiatives, Dr Meneses reminded the audience of the growing number of breast cancer survivors. Over 13.7 million people in the United States or 4% of the population have survived cancer. Of these, approximately 22% had breast cancer, making breast cancer survivors the largest group of cancer survivors in the United States. These numbers will only continue to grow; the National Cancer Institute (NCI) projects more than 18 million cancer survivors in 2022.
Dr Meneses then introduced navigators to the research approach that she and her team use when evaluating programs directed toward breast cancer survivors. These research efforts, known as behavioral studies, are led by multidisciplinary teams. Their goal is to determine if a given intervention, such as a multicomponent educational program, enhances patients’ long-term health and QOL. Using data from surveys and secondary databases, researchers document patient behaviors and health outcomes. They are ultimately looking for differences between women who participated in the educational program and women who did not.
With her colleagues at UAB, Dr Meneses has been involved with several NCI-sponsored behavioral studies. One of these studies, the Breast Cancer Education Intervention (BCEI), which was published in Oncology Nursing Forum in 2007,1 was recognized as a national model of cancer survivorship education. This randomized controlled trial of patient-directed, nurse-led QOL interventions was also cited in a 2012 Cochrane Database of Systematic Review’s article of psychosocial interventions to improve QOL. Notably, the BCEI study was the only one in the Cochrane review with nurse-led educational interventions that resulted in improved QOL.
The BCEI study, which was conducted in the early 2000s, targeted women in central Florida who were in their first year of survivorship after primary treatment for breast cancer. The primary study goal was to determine whether a 6-month program of nurse-led education and support affects patient-reported outcomes related to QOL.
Participants in the experimental arm of the study received the BCEI, which was delivered in 3 face-to-face sessions and 5 monthly follow-up sessions (3 by telephone and 2 in person). Those in the control group received 4 monthly attention control telephone calls and the BCEI at month 6.
When describing the educational sessions associated with the BCEI, Dr Meneses recalled, “Maintaining good contact and good communication made a huge difference. We nurses worked with patients to ensure that they called and talked to their physicians, talked to their oncology nurses, to their team, about health concerns that they had…. It is so important for nurse navigators to listen and really hear survivors’ specific needs.”
The 261 breast cancer survivors who participated in the BCEI study were primarily middle-aged with a median age of 54 years. Most were Caucasian, college educated, married, working full- or part-time, and had moderate family incomes. All had been treated with surgery, radiation, and/or chemotherapy at a regional cancer center that employed National Comprehensive Cancer Network guidelines and participated in breast cancer clinical trials.
The results of the BCEI study were highly encouraging. At 3 months, the experimental group reported improved QOL, whereas the control group reported a significant QOL decline. At 6 months, the experimental group reported continued maintenance of QOL. Although the control group also reported improved QOL, significant differences continued to exist between the 2 groups.
Dr Meneses summarized the key lessons learned in the BCEI study:
- Consistent support and education, “which we now call navigation,” makes a positive difference in the QOL of breast cancer survivors.
- Consistent support, education, and engagement of a motivated breast cancer survivor results in effective and long-term patient commitment to cancer surveillance and other health behaviors.
- This intervention required face-to-face contact, which is not inexpensive. Women in at-risk groups, including residents of rural areas of Florida and Spanish-speaking Latinas, were unable to participate in this program. These groups also deserve support and education.
“Just because you have a great study, a great intervention, so what if it is effective? Who even reads [these journals]? Our perspective is that you cannot hold on to effective evidence-based programs. You need to disseminate your work in ways that everyone can use.... How can we get these materials and this intervention into the hands of women who need it most?” Dr Meneses stated.
Dr Meneses shared details of 3 more recent “spin-off” projects that target at-risk breast cancer survivors. All of these programs were built using the framework of educational materials and interventions that had been proven in the BCEI study to enhance survivors’ QOL.
- Rural Breast Cancer Survivor (RBCS) Study: This study examined the effectiveness of a telephone-based, psychoeducational support intervention for rural breast cancer survivors. Working with the Florida Department of Health, the RBCS project used a population-based approach to recruit more than 500 breast cancer survivors living in rural Florida. Participants were randomized into an experimental and control group, and agreed to participate on a monthly basis for 12 months. The RBCS intervention is a multicomponent initiative consisting of individualized telephone education and support supplemented by written materials and tip sheets (English and Spanish). Education sessions focus on common problems faced by breast cancer survivors including cancer-related fatigue, lymphedema, and pain. Nurses teach participants about physical changes after breast cancer, how to live a healthy lifestyle (ie, physical activity, nutrition, diet), and about cancer surveillance and follow-up (ie, bone density testing, mammograms, gynecologic care, routine healthcare provider visits).
“Over 430 women have participated [in RBCS] over the past 4 years.… We are really excited about the dissemination potential of this project, which is now coming to a close.… Our preliminary results show that at-risk survivors benefit from survivorship support and education. These women are engaged as advocates for their care,” Dr Meneses said.
- Reach Out to Breast Cancer Survivors in North Central Alabama: In an initiative funded by the Komen Foundation, Dr Meneses and her colleagues targeted rural breast cancer survivors in Alabama. They adapted the educational materials used in the RBCS study, altering them from an eighth-grade to a fifth-grade reading level, and identified champions within identified Alabama counties. Dr Meneses noted that these champions were critical to the success of the Reach Out program, highlighting the example of a nurse and lymphedema specialist who passionately advocated for the program in her community near Birmingham.
- Young Breast Cancer Survivorship Network (YBCSN): According to the American Cancer Society, only 5% of all breast cancers diagnosed in the United States each year occur in women younger than 40 years of age. Dr Meneses stated that these young women often feel “invisible,” as patient support services, educational materials, and social networking sites typically target and depict middle-aged and older women. Recognizing that many of the young breast cancer survivors in Alabama are African American with triple-negative breast cancer, Dr Meneses and her colleagues performed a community assessment among this subpopulation to learn their specific concerns. The team also identified a program manager, a young survivor herself, who understands the needs of young women because she lived them personally.
YBCSN has grown to a network of 19 partners, including cancer centers, with a website (www.youngsurvivorsbhm.org) and the support of 2 national organizations, Living Beyond Breast Cancer and the Komen Foundation.
“We owe a debt of gratitude to breast cancer survivors. What we know today, as far as survivorship research and advocacy [across tumor types], is largely attributable to them,” Dr Meneses said.
Dr Meneses concluded her presentation by recommending the searchable database Research-Tested Intervention Programs (RTIPs). Supported by NCI and the Substance Abuse and Mental Health Services Administration, the RTIPs database (http://rtips.cancer.gov/rtips/index.do) allows healthcare professionals to access research-tested cancer control interventions and program materials, including materials used in the breast cancer intervention programs spearheaded by Dr Meneses.
The RBCS study and the YBCSN initiative offer timely and relevant demonstrations of the very real value associated with breast cancer care navigation. Dr Meneses explained, “[Navigators] are the heart of transitioning care for [breast cancer] patients and families.… You look into each patient’s future and say, ‘Here is where we would like to be. These are our benchmarks in the next 5, 10, 15, 20 years.’”
Three-Dimensional Nipple Tattooing
The second half of the breast cancer survivorship breakout session at the AONN+ conference focused on the growing use of 3-dimensional (3-D) nipple tattooing for patients with breast cancer who have undergone breast reconstruction. After recounting her personal experience with nipple tattooing, Lillie introduced Vinnie Myers, a self-taught tattoo artist from Finksburg, Maryland.
Vinnie gracefully thanked Lillie and the audience stating, “The fact that a tattoo artist is here [at your meeting] is a testament to how far tattooing has come. You must be on to something when Lillie Shockney introduces you!”
After leaving the Army, Vinnie opened a tattoo shop in a town north of Baltimore prepared to live out the American dream of owning a small business. In 2002, an unplanned encounter with a surgeon who performs breast reconstruction procedures for women who have undergone mastectomies, Vinnie’s life “changed forever.”2
Over time, and after study and experience, Vinnie has developed a technique of tattooing that recreates the shadowing and vasculature of a natural areola. Although the skin surface of the reconstructed breast is flat, his approach gives the appearance of a 3-D nipple.
“I think it is critically important that ladies complete themselves. What has been done in the past by nurses and doctors is not adequate. We need to change gears a little bit and think a little more artistically,” Vinnie stated.
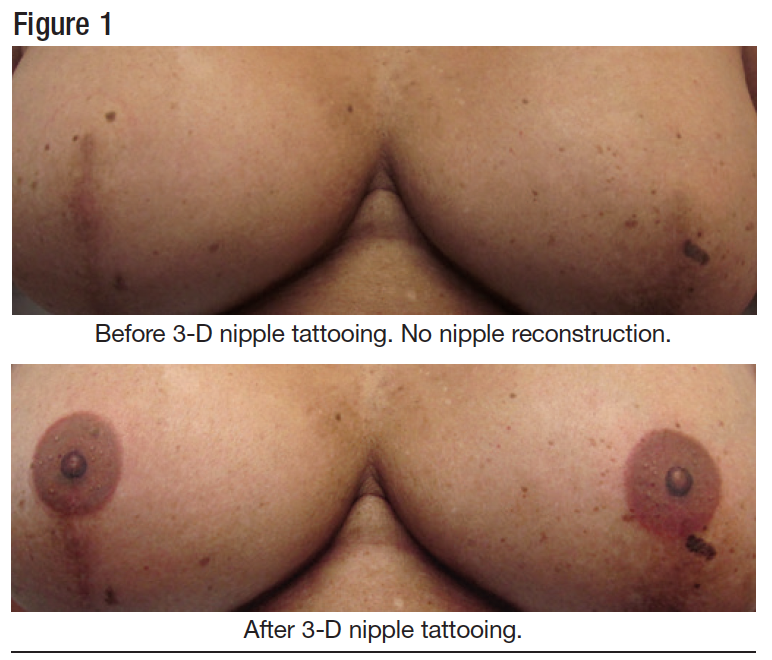
Using photographs to illustrate (Figure 1), Vinnie explained, “We create the illusion of projection where there is none.… This is the result that we would like to see on every woman who has breast reconstruction all over the world. It is a big task, but that is the mission.”
Traditional versus 3-D Nipple Tattooing
To illustrate the uniqueness of his nipple tattooing approach, Vinnie reviewed the history of nipple tattooing and the differences between “traditional” methods and his approach. He explained that plastic surgeons have approximately 2 hours of training during residency. Surgeons then train their nurses or medical aestheticians to perform tattooing after they have established their surgical practices, an approach to which Vinnie objects. “Why is it acceptable to have a nurse who has essentially zero training in tattooing do this final step of a reconstruction procedure?”
Vinnie also outlined “disconnects” in the tattooing equipment, including inks and dyes, and techniques used by the medical tattooing industry compared with the traditional tattooing industry. Because these groups have remained distinct, “There is no line of communication, no sharing of ideas [between medical and traditional tattoo artists].”
When talking about contrasts in artistic approaches used by surgeons performing tattoos relative to his personal approach, Vinnie clarified, “Let’s not take a washer, trace it, fill in the hole in the middle, and then tattoo that [on a breast]. This is an actual method being used right now by nurses and doctors in plastic surgery practices.”
Vinnie illustrated the results that he can achieve with one 3-D nipple tattooing session using an example of a patient with breast cancer who underwent a bilateral mastectomy (Figure 2).
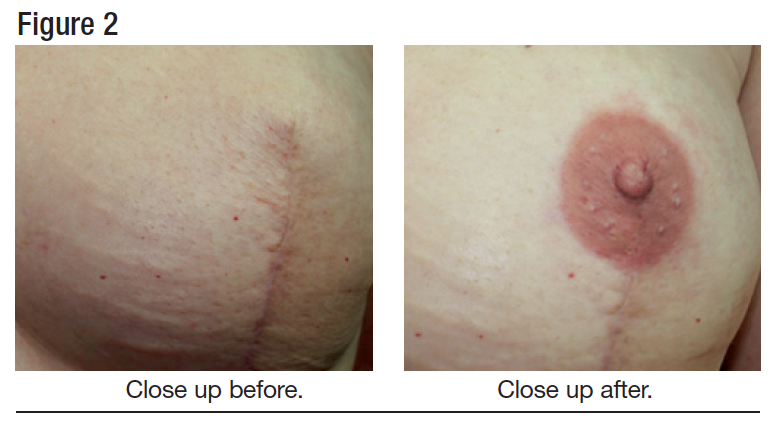
He noted that the patient underwent flap surgery, which resulted in a vertical scar that conveniently caused natural-looking projection of the breast tissue. While it rarely happens today, proactive communication among breast surgeons, plastic surgeons, and tattoo artists can ensure that the surgical procedures, including skin closures, are optimized for subsequent nipple tattooing procedures.
“The patient is happiest [when] everybody along the line communicates. Maybe it is a little more difficult, maybe it is a little harder to work that way. So what? The patient is happy in the end, which is what we are looking for,” Vinnie said.
Vinnie then compared dermabrasion nipple tattooing techniques with his tattooing method. Dermabrasion nipple tattoos use a high-frequency vibrating probe to push pigment into the skin. To achieve full color, several sessions may be needed. The range of colors available for dermabrasion can be limited and dermabrasion tattoos tend to fade over time. According to Vinnie, “[Dermabrasion] does not work. You are chopping up the dermis and you end up with scars. That tissue regenerates and pushes the pigment out. Very little pigment gets to the dermis, which is where you need it for good retention.”
FAQs for Oncology Navigators and Patients with Breast Cancer
Who is a candidate for 3-D nipple tattoos? Vinnie explained that all breast reconstruction patients are candidates for 3-D nipple tattoos: unilateral, bilateral, deep inferior epigastric perforator flap, stacked flap, and silicone gel implants.
When can a patient receive a tattoo? Vinnie recommends at least a 5-month window between the final breast reconstruction surgery and nipple tattooing, presuming the scar tissue is in the center of the breast. “Not 3 months, not 2 months, not what they’ve been telling you before.” Waiting at least 5 months allows tissue to heal and ensures good pigment retention.
If the procedure included expander exchange using an inframammary fold incision, such that there is no scar across the center of the breast, a 3-month time delay is viable.
What are the dangers in nipple tattooing? Based on his experience to date, Vinnie highlighted several challenges associated with nipple tattooing and patient selection. Skin quality, tissue depth, and scarring due to surgery and radiation are just some of the factors that affect aesthetic outcomes of 3-D nipple tattooing procedures. He noted, however, that this body of knowledge is evolving; “I am learning more and more that there is a whole lot to this [process]. This is a real procedure that needs to be addressed and approached just like any other procedure. We are trying to work out all the bugs so that the end result is optimal for the patient.”
Should the patient undergo nipple reconstruction? Nipples can be tattooed regardless of prior nipple reconstruction. The most important question for the patient is whether they prefer nipple projection. Vinnie argued that optimal aesthetic results are achieved when the patient does not undergo nipple reconstruction.
“It looks real to have areola tattoos with 3-D Montgomery glands, if you want them. That is not a problem. But the asymmetry that’s created, the unusual shapes, the flattening, the lack of flattening [with nipple reconstruction]; those play a part in what will look realistic. I do not recommend [nipple reconstruction], but it is really up to the patient,” Vinnie commented.
Can failed nipple tattoos and nipple reconstruction tattoos be fixed? Yes! Pointing to photographs of a failed nipple reconstruction (Figure 3), Vinnie explained that the patient has had one nipple flatten while the other has not. Using the 3-D technique, he was able to make both nipples appear to be the same size and projecting.
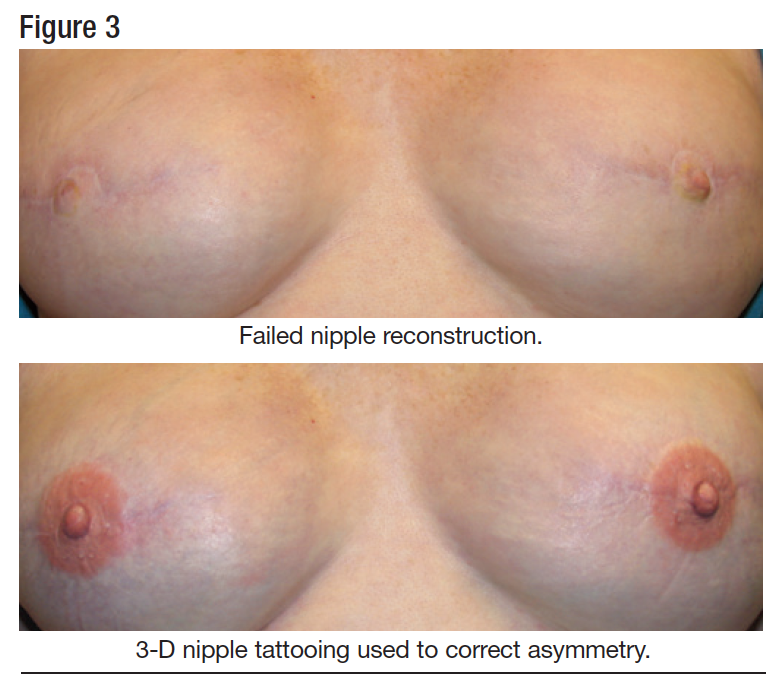
Vinnie illustrated his work using photographs of a patient with a unilateral breast and nipple reconstruction. The nipple tissue was scarred from the previous surgery and tattoo. “With not a whole lot of work, you can get a result that looks good, even after the patient has had a really bad tattoo and a really bad nipple reconstruction.”
“The bottom line is, a really bad reconstruction can look so much better with a good tattoo. And a really good reconstruction can look horrible with a bad tattoo.… You have to think ahead. Who do I want to go to? How do I want to go about it? Do I want nipple reconstruction?” Nurse navigators can help women learn about these options and consider these important questions.
How do you find a tattoo artist? Only a handful of tattoo artists claim to be experienced in 3-D nipple tattooing, including Vinnie Myers. “3-D tattooing is still relatively new. You are not going to be able to find somebody in every state who does it. It is just not that readily available. I am going to work my heart out to change that.”
Vinnie’s advice to patients and navigators was to explore the subject with respectable local tattoo artists, keeping in mind the following:
- Finding a respectable tattoo artist and shop is not difficult today. “Modern tattoo shops are not like the ones that your granddad visited when he was in the Navy. What you should expect is an edgy but professional, clean shop.”
- Ensure that the shop uses “universal precautions,” including an autoclave that has recently been spore tested. “If you ask about universal precautions and they have no idea what you’re talking about, go back to your car.”
- Look at photographs and examples of their work. Ask for referrals to people who they have tattooed, and talk with those people about their experience.
Vinnie reminded the audience that higher costs do not translate to better-quality nipple tattoos. Vinnie charges $400 for a unilateral nipple tattoo and $600 for bilateral tattoos, a price that he characterized as “reasonable.”
Is the cost of nipple tattooing reimbursed? Vinnie indicated that insurances that pay for nipple tattooing typically reimburse half of the artist’s fee. However, the payment process is not simple or straightforward. “They always kick it back. You have to stay with it. You have to be willing to submit the paperwork.” Vinnie and his office personnel are currently developing a “form letter” for submission to payers that includes all relevant terminology to facilitate reimbursement.
Vinnie concluded his portion of the Breast Cancer Navigation and Survivorship presentation by thanking Lillie and the audience for their interest in and support of his efforts. He reiterated his goal: to ensure that all women who undergo breast reconstruction have the opportunity to consider 3-D nipple tattooing that is performed by trained professionals. “With Lillie on my side, I think I have the best advocate. We are going to get something going!”
References
- Meneses KD, McNees P, Loerzel VW, et al. Transition from treatment to survivorship: effects of a psychoeducational intervention on quality of life in breast cancer survivors. Oncol Nurs Forum. 2007;34(5):1007-1016.
- Vinnie Myers: Tattoo artist Vinnie Myers, making breast cancer survivors whole again. Washington Times. October 25, 2013. http://communities.wash ingtontimes.com/neighborhood/metro-news/2013/oct/25/tattoo-artist- vinnie-myers-making-breast-cancer-su/#ixzz2q2R1BcVz. Accessed January 27, 2014.




